Abstract
Background: Rituximab-containing chemoimmunotherapy (R-CHOP) is a standard treatment for patients with diffuse large B cell lymphoma (DLBCL), with a high response rate. Achievement of only a partial response (PR) was regarded as treatment failure, but data on their prognosis are limited to date. Distinguishing PR from CR is not always clear because of controversies in interpreting 18-fluorodeoxyglucose positron emission tomography (FDG-PET) in rituximab-era. Recent advances have prompted a revision in the response criteria, as recently suggested at the 12th International Conference of Malignant Lymphomas (ICML), emphasizing the prognostic significance of FDG-PET results interpreted using the five-point Deauville score. Based on such changes, the prognosis of PR patients should be re-evaluated.
Patients and Methods: We conducted a retrospective multicenter study on behalf of the Consortium for Improving Survival of Lymphoma (CISL), to investigate survival outcomes and to define prognostic factors for PR patients after first-line treatment. A total of 758 patients with histologically proven DLBCL, who received the R-CHOP regimen between January 2005 and December 2013, were assessed. Among them, patients who achieved a PR defined by both computed tomography (CT) and FDG-PET at the end of R-CHOP were included in further analysis. Clinical information at diagnosis and after treatment was collected to determine the prognostic factors affecting the clinical outcome of PR patients. FDG-PET scans were reviewed by physicians and nuclear medicine experts in each institution and interpreted using the Deauville five-point scale. The prognostic role of secondary International Prognostic Index after R-CHOP (IPI2), assessed by restaging, age, performance status, residual multiple extranodal involvements and lactate dehydrogenase (LDH) levels, was evaluated. Progression-free survival (PFS2) and overall survival (OS2), measured from the date of the response assessment after R-CHOP to further progression or death, were determined by Kaplan-Meier methods with log-rank test. We also performed t-tests, χ2 tests, and Cox proportional hazard analysis. Statistical significance was accepted when two-sided p values were <0.05.
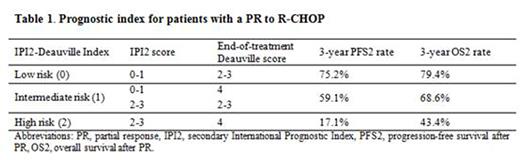
Results: In total, 88 (11.6%) patients partially responded to R-CHOP with a median age of 53.5 years were searched. Over a median follow-up of 47.8 months, 3-year PFS2 and OS2 rates were 58.8% and 69.4%, respectively. The IPI2 scores were 0-1 (low) in 68.2% and ≥2 (high) in 31.8% of patients. The Deauville scores after R-CHOP were 2-3 (low) in 57.9% and 4 (high) in 42.0% of patients. High (≥2) and low (0-1) IPI2 groups represented 28% and 72% of 3-year PFS2 rates (p <0.001). Patients with Deauville score 4 were also associated with worse 3-year PFS2 rates than those with a lower score (2-3) (40.4% vs. 71.1%, p=0.009). For OS2, IPI2 (47.6% vs. 77.7%, p=0.013) and Deauville score (57.5% vs. 75.3%, p=0.067) were prognostic, although the effect of the Deauville score was not statistically significant. A high-risk group, defined by the IPI2-Deauville index (Table 1), showed significantly lower 3-year rates of PFS2 (17.1% vs. 69.3%, p<0.001) and OS2 (43.4% vs. 75.1%, p=0.006) compared with other groups (Figure 1). In a multivariate analysis, the IPI2-Deauville index was an independent prognostic factor for disease progression (HR 1.76, 95% CI 1.15-2.69, p=0.009), adjusted with initial IPI score and bone marrow involvement at diagnosis. For OS2, the index did not remain significant in a multivariate analysis.
Conclusion: Our data shows that patients with DLBCL who achieved a PR to R-CHOP is still a heterogeneous group, and IPI2 and Deauville scores can be useful prognostic factors in addition to initial IPI at diagnosis. Validation through future prospective study would be valuable.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal