Abstract
Background:
The impact of time from diagnosis to chemotherapy initiation (time to treatment, TTT) for AML has been a topic of ongoing debate. A prior study reported that TTT ≥5 days adversely impacted overall survival in younger (<60 years of age), but not older (≥60 years of age), patients. However, subsequent studies found either no effect of TTT on overall survival, regardless of age, or an adverse impact of TTT on overall survival for both younger (>10 days) and older patients (>5 days). Prior data also showed no impact of TTT on early mortality. Given these conflicting findings, consensus on the impact of TTT on survival is lacking and warrants further study. Using prospectively collected population-based data, we analyzed a large cohort of adult AML patients to examine the effect of TTT on overall survival.
Methods:
Using data from the California Cancer Registry and Patient Discharge Dataset between 1999-2012, patients≥15years diagnosed with de novo AML and who received inpatient treatment between 1-90 days from diagnosis were identified (n=5337). Multivariable logistic regression was used to determine factors associated with TTT>5 days vs 1-5 days with data presented as odds ratios (OR) and 95% confidence intervals (CI). The effect of TTT on overall and 60-day survival was estimated using multivariable Cox proportional hazards regression with TTT (1-5, 6-10,>10 days)considered as a time-dependent variable. Patients were stratified by age group (<60,≥60 years) for all analyses.Multivariable models accounted for age, race/ethnicity, sex, number of comorbidities, marital status, neighborhood socioeconomic status, health insurance type, treatment at National Cancer Institute designated (NCI) vs non-NCI designated facility, use ofleukapheresis, and year of diagnosis.
Results:
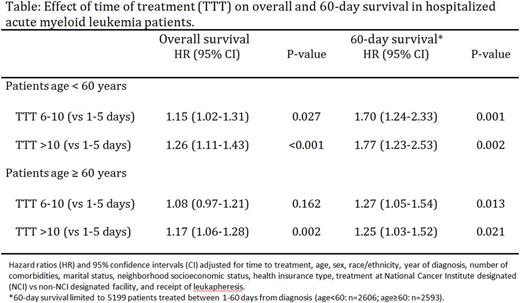
Of the 2659 patients <60 years of age, 61.0% were treated within 5 days and 79.7% within 10 days of diagnosis, compared to 43.8% and 65.0%, respectively, of the 2678 patients≥60 years of age. Patients≥60 years were more likely to have 3+ comorbidities compared to the younger age group (43.3% vs 25.9%, P<0.001). The likelihood of TTT>5 days increased with age in both younger and older patients. Across both age groups, patients requiringleukapheresis(age<60: OR 0.19, CI 0.10-0.34; age≥60: OR 0.23, CI 0.12-0.45), treated at a non-NCI (vs NCI) center (age<60: OR 0.62, CI 0.52-0.73; age≥60: OR 0.64, CI 0.52-0.78) and with 1-2 (vs 0) comorbidities (age<60: OR 0.81, CI 0.67-0.98; age≥60: OR 0.69, CI 0.54-0.88) or 3+ (vs 0) comorbidities (age<60: OR 0.77, CI 0.62-0.97; age≥60: OR 0.52, CI 0.41-0.66) had a lower odds of TTT>5 days. Younger (age<60) African Americans (vs non-Hispanic whites) had a higher odds of TTT >5 days (OR 1.43, CI 1.04-1.97). Delaying chemotherapy >10 days (vs 1-5 days) adversely impacted overall survival in both age groups (age<60: HR 1.26, CI 1.11-1.43; age≥60: HR 1.17, CI 1.06-1.28) (Table). However, TTT of 6-10 days (vs 1-5 days) affected overall survival in young (age<60: HR 1.15, CI 1.02-1.31), but not older patients. A TTT of 6-10 days (vs 1-5 days) adversely impacted 60-day survival in both age groups (age<60: HR 1.70, CI 1.24-2.33; age≥60: HR 1.27, CI 1.05-1.54); 60-day survival results were similar for a TTT >10 days (vs 1-5 days) (Table).
Conclusions:
In a large cohort of patients with de novo AML, TTT of up to 10 days did not have a negative impact on overall survival in patients over the age of 60. In younger patients (<age 60), TTT >5 days was associated with decreased overall survival. Delaying chemotherapy over 5 days adversely impacted 60-day survival in both age groups. Our observation that patients were more likely to have a shorter TTT at non-NCI designated hospitals may relate to delays associated with transfer to or clinical trial enrollment at NCI centers. Our results suggest that waiting to get results of ancillary testing, such as cytogenetic and molecular mutation analyses, in order to inform treatment decisions for AML patients, may be feasible in some patients with AML. In an era of rapidly evolving prognostic and treatment landscapes for AML, our findings may have implications for personalized therapy, including novel targeted therapies, and clinical trial design for patients withAML.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal