Abstract

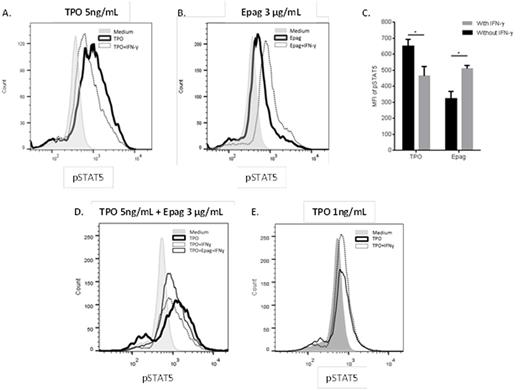
Thrombopoietin (TPO) is the main regulator of hematopoietic stem and progenitor cell (HSPC) self-renewal and survival. Upon binding to its receptor, c-MPL, TPO activates cell signaling, through JAK-STAT and other pathways, which is tightly balanced by negative regulatory signaling processes. Recent studies indicate that chronic exposure of HSPCs to IFNγ, as exemplified in subjects with severe aplastic anemia (SAA), impairs self-renewal by perturbing TPO signaling pathways. Despite elevated levels of TPO in subjects with SAA, the TPO receptor agonist Eltrombopag (Epag) improves trilineage hematopoiesis in refractory SAA, suggesting that it may activate signaling within HSPC in a way that is distinct from TPO under inflammatory conditions. To address the paradox of Epag efficacy despite high endogenous TPO levels in bone marrow failure, G-CSF mobilized human CD34+ cells from 6 healthy donors were cultured in the presence of SCF, FLT3 and either TPO 5 ng/ml (TPO5) or Epag 3 μg/ml (Epag), with or without IFNγ 100 ng/ml. After 7 days in culture, cells were characterized via flow cytometry, CFU assay and transplantation in immunodeficient (NSG) mice. The percentages of CD34+ cells in cultures containing TPO5 or Epag alone were similar (83.3 ± 9.7% and 87.6 ± 7.1%, respectively), but were better preserved with Epag than TPO5 in the presence of IFNγ (46.7 ± 16.1% and 24.6 ± 15.0% respectively, p<0.05). Accordingly, when comparing 7-day cultures with and without IFNγ, the absolute numbers of CD34+ cells were markedly reduced with TPO5 (average 7.6-fold, p<0.005) but only minimally decreased with Epag (average 1.6-fold, p = n.s.). The adjusted numbers of CFUs after 7 days in the presence of IFNγ similarly decreased 2.7-fold with TPO5 but remained unchanged with Epag compared to cultures without IFNγ. When the 7-day expanded progeny of an equal starting number of CD34+ cells was transplanted in NSG mice, human cell engraftment was superior with Epag (34 ± 3.8% human CD45+ cells) than with TPO5 (21 ± 1.8% human CD45+ cells, p<0.05) cultures in the presence of IFNγ, suggesting an impact of Epag on the most primitive long-term repopulating HSPCs. To investigate potential mechanisms by which Epag positively affects maintenance of HSPCs under inflammatory conditions, we examined cell signaling pathways induced upon binding of TPO, Epag and IFNγ to their respective receptors in human CD34+ cells. At a concentration of 5ng/mL, TPO induced a rapid (peak < 1 hour) and high potency rise in STAT5 phosphorylation followed by a rapid (< 2 hours) decay in signal. In contrast, Epag induced a slow (peak 4 hours) low potency rise in STAT5 phosphorylation, and the signal persisted for at least 10 hours. The difference in cell signaling potency and kinetics between TPO and Epag is likely related to their binding to distinct regions of c-MPL, resulting in alternate receptor conformational changes. We next investigated the impact of IFNγ on TPO and Epag-induced STAT5 phosphorylation at the signal peak (<1 and 4 hours, respectively). As previously shown in murine HSPCs, IFNγ impaired TPO signaling in human HSPCs (Figure, panels A, C). In contrast, Epag-induced STAT5 phosphorylation was preserved or increased in the presence of IFNγ (Figure, panels B, C). When Epag and TPO were combined, inhibition of TPO signaling by IFNγ was partially restored (Figure, panel D). By reducing the dose of TPO from 5 to 1ng/mL, and therefore reducing the potency of signaling to levels similar to Epag, the inhibitory effect of IFNγ on TPO signaling was abolished (Figure, panel E). Activation of IFNγ receptor by its ligand induces phosphorylation of STAT1 and subsequent expression of suppressor of cytokine signaling-1 (SOCS-1), a negative regulator of both IFNγ and c-MPL receptors via inhibition of STAT1 and STAT5 phosphorylation, respectively. We found that IFNγ-induced phosphorylation of STAT1 was increased in the presence of TPO 5ng/mL (1.5-fold increase, p<0.05) but unaffected by Epag (1.1-fold increase, p = n.s.) or TPO 1ng/mL (1.1-fold increase, p = n.s.). Our data indicate that Epag counters IFNγ-induced perturbation of TPO signaling in human HSPCs. Epag produces an unopposed low potency, slow kinetic positive signal and activates c-Mpl above a threshold level critical for HSPC self-renewal. Epag's evasion of IFN blockade of a critical pathway of growth factor cell signaling may explain its efficacy in improving hematopoiesis in SAA.
Cheng:Novartis: Research Funding. Cheruku:Novartis: Research Funding. Alvarado:Novartis: Research Funding. Cash:Novartis: Research Funding. Dunbar:Novartis: Research Funding. Young:Novartis: Research Funding. Larochelle:Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal