Abstract

Introduction. Multiresistant (MR) bacteria colonization is considered predictive of related bloodstream infections (BSI), which are worrisome among hematological patients (pts). Few data are available about the actual incidence of MR colonization and the probability of developing a BSI in this population. A multicentric prospective observational study has been carried out within the SEIFEM group, with the aim of detecting the incidence of MR bacterial colonization and the probability of developing MR BSI in hematological pts.
Patients and Methods. Between March 1st and August 31st 2015, all pts with a hematological neoplasm admitted to 18 Italian Centres participating to SEIFEM were screened for MR colonization with a rectal swab; cultures of other sites were performed if clinically indicated. Patients showing MR bacterial colonization were recorded in a database where the occurrence of any BSI was correlated with age, gender, type and phase of disease, stem cell transplantation (SCT), presence of invasive devices, type of colonizing bacteria.
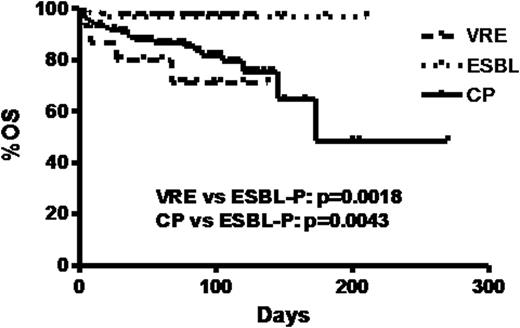
Results. During a 6-month period, 189 pts with MR colonization were observed. Incidence was 8.9% among all admissions (189/2122). Median age was 59y (range 0-89) and M/F ratio 116/73. Eighty-two pts were affected by acute leukemia, 75 by lymphoma, 24 by myeloma, 6 by chronic myeloproliferative/myelodysplastic syndromes and 2 by aplastic anemia. Forty-four pts underwent SCT (28 autologous and 16 allogeneic). Vancomycin resistant enterococci (VRE) were responsible for colonization in 15 (7.9%) pts, extended spectrum beta-lactamases producing (ESBL-P) enterobacteria in 80 (42.3%) and carbapenemase producing (CP) Gram-Negative Rods (GNR) in 108 (57.1%). Thirteen of 14 pts with multiple colonizations had both ESBL and carbapenemase producing enterobacteria. Multivariate analysis of risk factors for type of MDR colonization showed that a complete hematologic remission was associated to ESBL-P enterobacteria colonization, but protective for CP strains (OR 2, 1.1-3.7, p=0.02 and 0.43, 0.23-0.79, p=0.006, respectively). Overall, 62 pts (32.8%) colonized with MR bacteria developed at least one BSI during the period of observation; 36 of them (58.1%; 19% of the whole series) developed BSI by the same pathogen (MRrel-BSI) (2 VRE, 14 ESBL-P E. coli, 2 ESBL-P K.pneumoniae, 1 ESBL-P E. aerogenes, 12 CP K. pneumoniae, 3 CP P. aeruginosa and 2 CP Acinetobacter spp). The rate of MRrel-BSI according to antibiotic resistance was 13.3% for VRE colonization, 19.5% for ESBL-P enterobacteria and 17.6% for CP GNR. CP K. pneumoniae, but not other CP enterobacteria, was predictive of MRrel-BSI (26.7%). In 82% of cases, MRrel-BSI occurred during neutropenia. At multivariate analysis of predictors of BSI, a relapsed/refractory hematological disease was associated to MRrel-BSI (OR 3.1, 1.4-6.7, p=0.005). Unrelated BSI were also observed in 32 pts (51.6%; 16.9% of the whole series), including 6 MR BSI (2 CP P. aeruginosa, 3 CP K. pneumoniae and 1 VRE). After a median follow-up of 80 days (range 0-270), 25 pts died (13.2%). Three-month overall survival (OS) of the entire cohort was 86%±2.9SE, being significantly lower for pts colonized with VRE (71%) and CP (82%) in comparison with those colonized with ESBL-P bacteria (97%, p=0.0018 and 0.0043 respectively) (Fig.1). Death was attributable to CP GNR related BSI in 5 pts and to VRE related BSI in 1. Multivariate analysis showed that CP GNR related BSI (OR 8.3, 2.2-30.5, p=0.001) and VRE related BSI (OR 87.9, 1.1-675.9, p=0.04), together with intensive care unit admission (OR 50.6, 4.5-570.9, p=0.001) were independent predictors of mortality at 30-days from known colonization, whereas having disease in complete remission was protective (OR 0.02, 0.001-0.43, p=0.01).
Conclusions. Incidence of MR colonizing bacteria, particularly ESBL-P and CP GNR, affects nearly 10% of italian hematological cancer pts and results in a MRrel BSI in about one fifth of cases, mainly during neutropenia. MRrel-BSI are responsible for more than 50% of BSI observed in MR colonized pts and are significantly more frequent in relapsed/refractory hematologic disease. VRE and CP GNR colonizations but not ESBL-P are associated to lower OS and predict for a higher fatality of related BSI. Among CP enterobacteria, only K. pneumoniae is associated with MRrel-BSI. Empiric antibiotic treatment should be better tailored taking into account these results.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal