Abstract
Introduction: The prevalence of silent stroke increases monotonically with age in SCD patients, with more than 50% developing detectable white matter hyperintensities on MRI by adulthood. We are exploring the use of inhaled oxygen as a contrast agent to try to identify individuals at risk for silent stroke and to better understand how the brain regulates its own oxygen delivery. In this study, we report changes of brain Blood Oxygen Level Dependent (BOLD) signal and frontal Near Infrared Spectroscopy (NIRs) to 5 minutes of inhaled 100% oxygen in patients with sickle cell disease (SCD), non sickle anemia (ACTL), and control subjects.
Method: The study was approved by the institutional review board and performed at Children's Hospital Los Angeles (CHLA); all patients provided informed consent. Patients with previous stroke, pregnancy, and acute chest pain and crisis hospitalization within one month were excluded. 19 SCD patients (age = 20.7 ± 8.8), 12 patients with non sickle anemia syndromes (age = 25.1 ± 6.9) and 20 ethnicity matched control (CTL) subjects (age = 30.5 ± 12.7) were studied. Peripheral oxygen saturation (SpO2%) was measured by MRI compatible pulse oximeter. A five minute BOLD sequence was acquired with the patient breathing room air for 50 seconds, followed by 100% oxygen for 250 seconds. NIRS recordings of oxygenated hemoglobin change (DOHB), deoxygenated hemoglobin change (DDHB) and tissue oxygenation index (TOI) were recorded from the patient's forehead. Average BOLD signal was from a 6 cm slab in the middle of the brain. CBC, hemoglobin electrophoresis, and markers of hemolysis were also measured.
Results: A representative frontal DOHB signal, and the parameters used to characterize its time-course, are shown in Figure 1. DOHB remained stable until oxygen was administered and then increased over several minutes to a maximum. In many patients, the DOHB signal subsequently declined back toward baseline, representing the effects of compensatory cerebral vasoconstriction. The delay time was shorter in anemic subjects because of increased cerebral blood flow, but the rise times were not different. Peak DOHB increase was greater in SCD patients than in ACTL or non anemic control subjects (1.4 mM ± 0.2mM, 0.8 mM ± 0.2 mM and 0.6 mM ± 0.4 mM, respectively, p <0.0001 by ANOVA). There was no difference in the DOHB vasoconstriction response among the three patient groups.
DOHB was highly correlated with DDHB and DTOI in all three patient groups. Consequently, both DDHB and DTOI changes were also larger in SCD patients. All three NIRs signal changes were larger in non-transfused SCD patients than in patients on chronic transfusions. Non-transfused SCD patients had more significant increases in SpO2% than chronically transfused subjects and the effect was proportional to hemoglobin F%, suggesting a p50 effect. After controlling for SpO2%, SCD patients still exhibited larger NIRs changes than ACTL or CTL patients, but the differences between transfused and non transfused SCD patients disappeared.
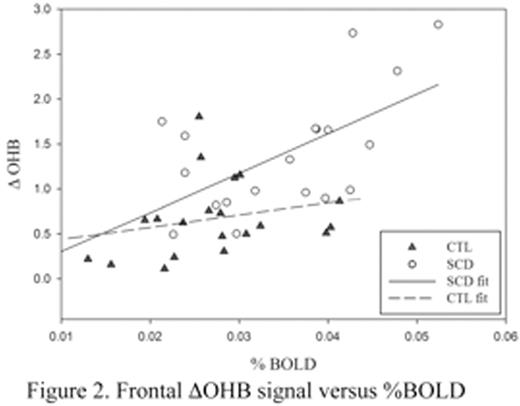
Whole brain %BOLD was also correlated with changes in DOHB, DDHB, TOI, and SpO2%. The relationship between DOHB versus %BOLD is illustrated in Figure 2. %BOLD changes were also significantly higher in SCD patients. However, unlike the NIRS changes, whole brain %BOLD differences could entirely be explained by differences in SpO2% with hyperoxia.
Conclusion:100% oxygen administration increases brain oxygenation in SCD patients to a greater degree than in control subjects or patients with anemia of other etiologies. Some of the differences can be explained by differences in resting oxygen saturations but disparities between BOLD and NIRs response suggest regional variation of brain oxygenation in response to this challenge.
Wood:Apopharma: Consultancy; AMAG: Consultancy; World Care Clinical: Consultancy; AMAG: Consultancy; Celgene: Consultancy; Apopharma: Consultancy; Biomed Informatics: Consultancy; Celgene: Consultancy; Ionis Pharmaceuticals: Consultancy; Vifor: Consultancy; Vifor: Consultancy; Ionis Pharmaceuticals: Consultancy; Biomed Informatics: Consultancy; World Care Clinical: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal