Abstract
Introduction: Tyrosine kinase inhibitors (TKIs) have been shown to be efficacious for the treatment of chronic myeloid leukemia (CML). However, resistance, lack of response, or intolerance may occur, resulting in disease progression. There is a paucity of evidence quantifying the real-world healthcare burden of patients with CML progression. Thus, the objective of this study was to evaluate the economic consequences of patients with CML progression using a real-world database analysis.
Methods: Patients (≥18 years of age) with at least 1 inpatient or ≥2 outpatient (≥30 days apart) diagnoses of CML were identified from the MarketScan Commercial and Medicare healthcare claims databases between January 1, 2007 and June 30, 2015. CML patients were grouped into 2 study cohorts, those with evidence of disease progression and those without. Patients with CML progression were identified by the presence of claims for acute myeloid leukemia (AML)-like or acute lymphoblastic leukemia (ALL)-like chemotherapy treatments, based on the guidelines of the National Comprehensive Cancer Network (version 1.2016), or a hematopoietic stem cell transplant (HSCT). For patients with progression, the first date of such a claim was defined as the index. For patients without evidence of progression, a random date after the first CML diagnosis was identified as the index date. In order to increase accuracy of detecting progression, patients with other cancers, including AML and ALL, documented prior to the first recorded diagnosis of CML were excluded from the study. Patients were required to have continuous medical and prescription insurance coverage during the 12 months prior to the index date (baseline period). Demographics and clinical characteristics were evaluated during the baseline period. Healthcare resource utilization, including hospitalizations, outpatient medical services, and outpatient prescription drug usage, and the associated costs were captured during the baseline period and a variable follow-up period, lasting ≥1 day and up to 1 year, and compared among study cohorts. All costs were inflation adjusted to 2015 cost level. Generalized linear models (GLMs) were used to further compare the incremental costs of CML patients with vs. without progression while adjusting for various factors.
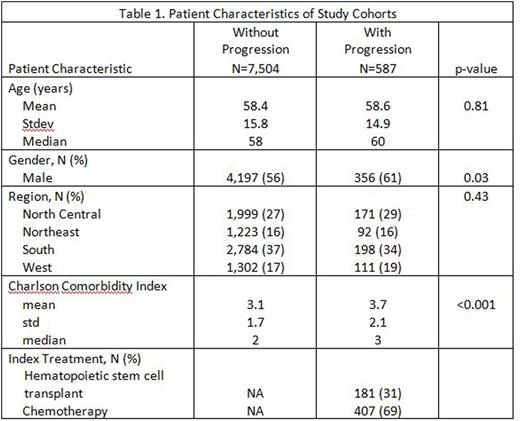
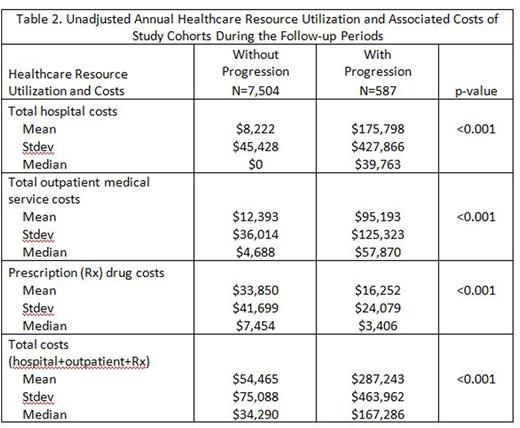
Results: Of the overall identified CML study population, 587 (7%) experienced disease progression and 7,504 did not. A greater percentage of male than female patients had evidence of disease progression and CML patients with progression had more comorbidities, as measured by Charlson Comorbidity Index, than those without progression (Table 1). Approximately 31% of CML patients with progression were treated with HSCT at the index date, while 69% were treated with chemotherapy (Table 1). During the baseline period, mean total healthcare costs, including costs for hospitalizations, outpatient medical service costs, and outpatient prescription costs were significantly greater for CML patients with vs. without progression ($143,778 vs. $53,143, p<0.001). During the follow-up, mean total annual healthcare costs, costs for hospitalizations, and outpatient medical service costs, were substantially greater for patients with vs. without progression; however, costs for outpatient prescription drugs were less (Table 2). When patient characteristics were taken into consideration with a GLM, the incremental costs for CML patients with vs. without progression were $270,925 (CI: $235,290, $311,958, p<0.001); when an additional GLM model was used, in which the baseline healthcare costs of CML patients were added as a covariate, the incremental costs for patients with vs. without progression were $136,308 (CI: $119,223, $155,841, p<0.001).
Conclusions: The healthcare burden, in terms of healthcare resource utilization and costs, of patients with CML progression is substantial. Healthcare providers and payers need to consider various strategies to minimize the rate of CML progression.
Elias:Bristol-Myers Squibb: Consultancy. Lin:Bristol-Myers Squibb: Consultancy; Novosys Health: Employment. Siegartel:Bristol-Myers Squibb: Employment. Lingohr-Smith:Novosys Health: Employment. Menges:Novosys Health: Employment. Makenbaeva:Bristol-Myers Squibb: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal