Abstract
Background:
Patients with acute myeloid leukemia (AML) often experience lengthy inpatient admissions resulting from toxicity from the disease and chemotherapy. There are limited data on which factors are associated with longer hospitalizations. We examined hospital and patient characteristics associated with length of stay (LOS) for adults with AML using a large US national database.
Methods:
We extracted admission data for patients with AML and myeloid sarcoma from the 2012 Healthcare Cost and Utilization Project National Inpatient Sample (HCUP-NIS). Due to the skewed distribution of data, multivariable negative binomial regression was used to test the association of the following factors with LOS: age, sex, region (Northeast NE, Midwest MW, South, West), income, insurance, hospital type, number of chronic conditions, and death. Separate models were built for non-elderly (age <60 yrs) and elderly (≥60 yrs) AML patients to estimate rate ratios as a percent increase or decrease in LOS. We assessed significance p<0.05 of the following interactions: hospital type*region, hospital type*chronic conditions, hospital type*death, and region*race. All results apply the HCUP-NIS weights.
Results:
There were 44,650 admissions associated with AML in 2012. Median patient age was 64 yrs (Interquartile Range, IQR 51-73), with 62% ≥ age 60. Nearly half (45%) were female. Median LOS for the entire cohort was 6 (IQR 3-18) days.
Age < 60:
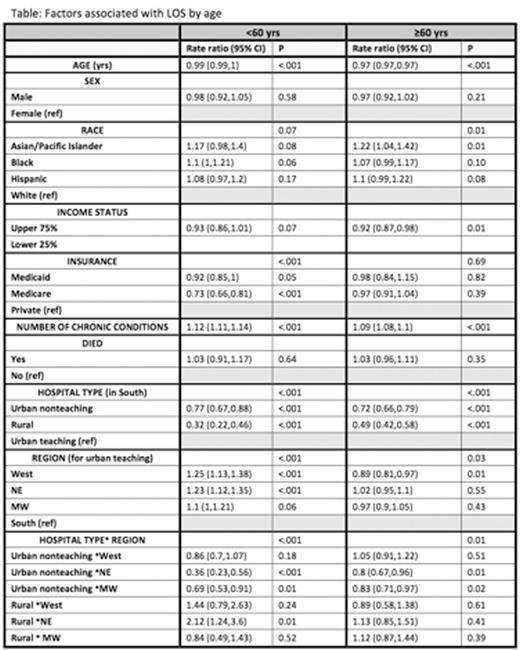
Median LOS was 7 (IQR 4-25)days. Median age was 47 yrs. In multivariate analysis, older age and Medicare were associated with shorter LOS (Table). More chronic conditions were associated with longer LOS: there was 12% longer LOS for each additional chronic condition. We found an interaction between hospital type and region. Within the South, admissions to urban teaching hospitals had longer LOS than to nonteaching and rural hospitals. Admissions to urban teaching hospitals were associated with longer LOS in the West and NE than the South.
Age ≥60:
Median LOS was 5 (IQR3-13) days. Median age was 71 yrs. Older age and higher income were associated with shorter LOS, while more chronic conditions were associated with longer LOS (Table). Asians had longer LOS than whites. We found an interaction between hospital type and region. Within the South, urban teaching hospitals had longer LOS than nonteaching and rural hospitals. Urban teaching hospitals had shorter LOS in the West than South.
Conclusions:
For both age groups, younger age, more chronic conditions, and the hospital type by region interaction were associated with longer LOS. Income and race affected LOS only in the elderly, whereas insurance affected LOS in the <60 yrs. The impact of hospital type on LOS varied by region and differently within each age group. These differences suggest that hospital practices vary by region, hospital type, and patient demographics. The clinical implications of these findings warrant further study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal