Abstract
Introduction
HLA-haploidentical hematopoietic stem cell transplant (Haplo HSCT) is a potentially curative strategy for patients lacking a HLA matched donor or a suitable unrelated donor. The use of post-transplant Cyclophosphamide (Cy) for GVHD prophylaxis and the particular characteristics of Haplo-HSCT can be linked to a higher risk of hemorrhagic cystitis (HC) and viral infections. In this context, our aim was to analyze HC in both haploidentical and conventional donor transplants in our center.
Material and Methods
We retrospective analyzed of 237 patients who received an HSCT in our center, between August-2012 and January-2016. We analyze the incidence of HC in the early post-HSCT period (6 months) and its characteristics in those patients receiving Haplo (n=36, 15%) and we compared it with a non-haploidentical donor transplant group from the same period (n=201, 85%).
Results
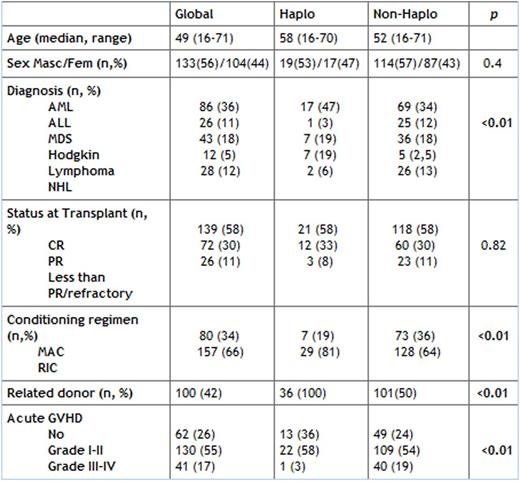
Patients' characteristics are summarized in table 1. Both groups are balanced, except for diagnosis due to the high proportion of Hodgkin lymphoma in Haplo group, conditioning regimen, and GVHD grade III-IV with a lower incidence in Haplo.
Conditioning regimen in Haplo consisted of Fludarabine (30mg/m2x or 50mg/kg x 4days in RIC or MA regimen) and Busulfan (3.2 mg/kg x 2 in RIC or 3 days in MA). Post-HSCT Cy was used for GVHD prophylaxis in 94%. Median of days to reach more than 500x10^9 granulocytes and more than 20x10^9 platelets in Haplo group were 18 (13-30) and 23 (0-103) respectively.
Hemorrhagic cystitis: Incidence of HC was 33% vs. 13% in conventional HSCT (p=0.03). Infectious etiology was documented in 84% of the Haplo recipients and 89% in conventional HSCT (p=0.87). In Haplo, HC was caused by BK/JC polyomavirus in 67% and adenovirus in 17%. Among conventional HSCT recipients, BK/JC was documented in 75% and adenovirus in 14% of HC. Viral infection was diagnosed by positive PCR in urine.
HC appeared at a median of 65 days post-HSCT (5-557), without differences between Haplo and non-Haplo: 61 (5-423) vs. 67 (8-557).
Treatment of HC consisted of hyper-hydration and spasmolytic drugs in 19 patients. Intravesical cidofovir was used in 7 and intravenous cidofovir was needed in 2 cases.
Receiving an Haplo HSCT was associated with a higher risk of developing HC [OR 3.5 (95% CI 1.56-7.91); p=0.002]. We did not observed association between HC and conditioning regimen (p=0.18), receiving ATG (p=0.45) or presence of acute GVHD grade I-II (p=0.75) or grade III-IV (p=0.46). Haplo donor was the only variable with significant impact in multivariate analysis.
Conclusions
Incidence of HC is higher in Haplo HSCT, being viral infections and not Cy toxicity, the main cause (polyomavirus BK/JC as the first cause).
Mateos:Janssen, Celgene, Amgen, Takeda, BMS: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal