Abstract
Background:Allogeneic hematopoietic cell transplantation is a cornerstone of therapy for hematologic malignancies and often a patient's only curative intent treatment. Following development of post-transplant cyclophosphamide (PTCy) regimens, the use of haploidentical hematopoietic cell transplantation (haplo-HCT) has expanded. While overall outcomes for haploidentical transplantation appear to be excellent, its novel approach brings toxicities that are particular to its biological and clinical milieu. We recently described occurrence of severe cytokine release syndrome (CRS) after haplo-HCT. We further reported that severe CRS was associated with poor clinical outcomes, including transplant related mortality (TRM), overall survival (OS), and neutrophil engraftment (Abboud et al, BBMT, 2016). However, the factors predicting the occurrence of and long-term outcomes of patients who develop severe CRS after haplo-HCT is currently not known.
Objective: To describe our clinical experience with CRS in an expanded cohort of haplo-HCT patients, its implication on clinical outcomes and elucidation of possible risk factors for the development of severe CRS.
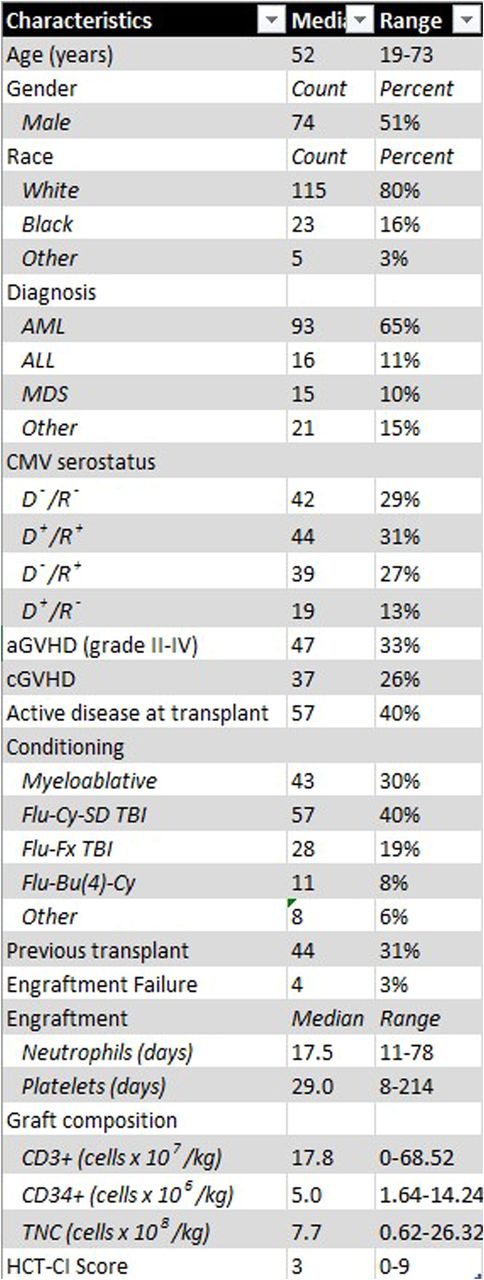
Patients and Methods: We performed a retrospective review of patients who had undergone peripheral blood T-Cell replete haplo-HCT with PTCy from July 2009 through March 2016 at our institution. A total of 137 patients were identified, 51% (74) were male, with a median age at transplant of 52 (19-73), a total of 40% (57) had active disease at the time of transplant. The most common diagnosis was AML (93 pts), followed by ALL (16 pts) and MDS (15 pts). Thirty-one percent (44 pts) had undergone prior transplant. In grading CRS, we used our approach modified from by Lee et al (Blood, 2014). Twenty-two patient, donor and disease characteristics were examined to identify predictors for the development of severe CRS.
Results:One hundred and twenty-four (90%) of patients met criteria for CRS, and 26 (19%) suffered from severe (grade 3-4) CRS. Virtually all patients (99%) with CRS suffered from fevers. Patients with severe CRS had a significant delay in neutrophil (p < 0.0001) and platelet (p < 0.0001) engraftment compared to the patients who developed mild or no CRS (Figure 1A and 1B). Severe CRS was also associated with a high early transplant related mortality; the rate of death before post-transplant day 28 was 6.9 times higher for patients with grade 3-4 CRS compared with those with mild CRS (p < 0.0001, Figure 1C). Consistent with these findings, the development of severe CRS was associated with extremely poor survival. Median survival was 3 months for grade 3-4 CRS, 15 months for grade 1-2 CRS, and 13 months for no CRS. One-year OS was 4% for grade 3-4 CRS, 55% for grade 1-2 CRS, and 50% for no CRS (Figure 1D). There was no difference in the cumulative incidence of relapse, acute graft versus host disease, and chronic graft versus host disease (data not shown). A total of nine patients received Anti-IL-6 Therapy with tociluzimab (4 mg/kg of actual body weight), 4 of which suffered from severe CRS.
In terms of predictive factors, the development of severe CRS was associated with disease risk index (p=0.037), HCT-CI score (p=0.005) and presence of a previous transplant (p=0.026) by univariate analysis. Risk and severity of CRS did not differ by age, ABO mismatch, age, CMV status of donor, donor sex, T-cell or CD34 cell dose. There was no difference in rates of CRS among patients in remission or with active disease at the time of transplant.
Conclusions: Severe CRS after peripheral blood haplo-HCT is associated with high early TRM, poor OS and delayed neutrophil and platelet engraftment. Furthermore, patients with high DRI, high HCT-CI and prior HCT are at a higher risk for the development of severe CRS after haplo-HCT. We have previously shown the safety and potential efficacy of using anti-IL-6 therapy in these patients. Our current results suggest potential benefit to targeting this pathway prophylactically in patients at high risk for the development of severe CRS.
CRS impacts neutrophil (A) and platelet (B) engraftment and is associated with high TRM (C) and poor OS (D).
CRS impacts neutrophil (A) and platelet (B) engraftment and is associated with high TRM (C) and poor OS (D).
DiPersio:Incyte Corporation: Research Funding. Abboud:Gerson and Lehman Group: Consultancy; Merck: Research Funding; Teva: Research Funding, Speakers Bureau; Novartis: Research Funding; Pfizer: Research Funding; Seattle Genetics: Research Funding; Alexion: Honoraria; Baxalta: Honoraria; Pharmacyclics: Honoraria; Takeda: Honoraria; Cardinal: Honoraria. Fehniger:Affimed: Consultancy; Celgene: Research Funding; Fortress Biotech: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal