Abstract
Background
Major ABO mismatch in allogeneic bone marrow transplant (BMT) can cause clinical problems like severe transfusion reactions, acute haemolysis, and delay of red blood cell (RBC) engraftment or manifestation of pure red cell aplasia, related to circulating isoagglutinin titers. Even there is no increased incidence of graft failure or slower engraftment of neutrophils and platelets ABO mismatch leads to an increase of transplant related mortality. To reduce circulating isoagglutinin titers pre transplant plasma exchange during conditioning period can be performed. This procedure can be wearing for the patient and rebound effects are observed. RBC depletion can cause a loss of CD34+stem cells in bone marrow. A further strategy to reduce circulating isoagglutinin titers is in vivo immunoadsorption due to donor type RBC transfusion pre transplant.
Aim of the study
The Aim of the retrospective single center study was to investigate the safety and tolerability of donor-type red blood cell transfusion prior to allogeneic stem cell transplantation in children with major ABO mismatch.
Methods
From 2007-2015 37 children (median age 7 years, range 0.6-18.4) received an ABO mismatched RBC transfusion (2-3 ml KG BW) pre transplant under antihistaminic and steroid cover. Reaction to donor type RBC and graft transfusion, number of donor type RBC transfusions, haemolysis parameters, and trend of isoagglutinin titers, and engraftment data were observed.
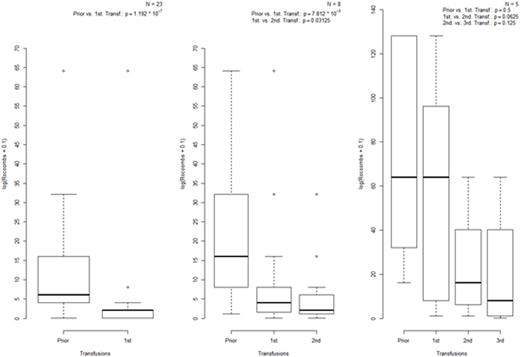
Wilcoxon signed-rank test was used to examine the difference between the paired values of titers (Conventional test tube, CTT; titration method using nonspecific anti-IgG antibody; Anti-IgG gel titer) before and after donor type RBC transfusion. Age and time until engraftment were reported using median and ranges. The quantitative values were reported using frequency and percentage. All statistical tests were two-sided with a significance level of 5%. Data analysis was performed using commercial software R.Statistical methods.
Results
Safety of mismatched RBC transfusions
Compared with accidentally transfused RBC no severe complications are observed in our cohort. 34 (92%) children presented no reactions (Grade 0), 1 child had a minimal oxygen demand,1 child showed a mild hypertension (Grade 1) and 1 child a moderate hypertension, requiring treatment. Neither severe reactions nor anaphylactic shock were observed.
Efficiency of mismatched RBC transfusion
A significant reduction of isoagglutinin titers was defined as a final titer of 1:4 or at least a reduction of 3 titer steps was achieved. 23 of 37 (64%) required 1 donor type RBC transfusion to reduce significant the isoagglutinin titers, 8 patients (22%) needed a second and 5 patients (14%) a third transfusion. Figure 1 showed the significant reduction of isoagglutinin titers in the different patients groups after donor type RBC transfusion. The pairwise analysis of isoagglutinin titers indicates that the initial titer of patients required one donor type transfusion of RBC was significant lower than in the patient group required 2 or 3 transfusions.
Engraftment data
The median time to WBC and platelet engraftment was 21.5 (range 19-24) and 28 (range 26-60) days respectively.
Haemolysis parameter post mismatched RBC transfusion
Haemolysis parameter lactat dehydrogenase (LDH) and bilirubin was determined on a daily base. In all patients no significant increase of bilirubin levels was observed.
Conclusion
Donor type RBC transfusion is a safe, tolerable and effective procedure to reduce the isoagglutinin titers prior to allogeneic ABO mismatched bone marrow transplantation in children. In our cohort no severe transfusion reactions, acute haemolysis, delay of engraftment or manifestation of pure red cell aplasia was observed.
Jarisch:Novartis: Consultancy. Bader:Novartis: Consultancy, Honoraria; Servier: Consultancy, Honoraria; Medac: Research Funding; Riemser: Research Funding; Neovii: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal