Abstract
Introduction: Hematological complete remission (CR) is the evident prognostic factor of allogeneic hematopoietic stem cell transplantation (HSCT) in patients with Acute Myeloid Leukemia (AML). CR with incomplete blood cell count recovery (CRi) after induction therapy was identified as independent prognostic factor for inferior long-term outcomes in patients with AML achieving remission (Chen et al, JCO 2015). There is a paucity of data regarding the impact of response (CR vs. CRi) prior to allogeneic HSCT. Here we examined whether CRi provide prognostic information on the transplant outcomes.
Methods: We retrospectively analyzed 73 consecutive adults with AML who received first allogeneic HSCT between 2008 and 2015. All clinical data were collected from medical records. CRi were defined CR with absolute neutrophil count < 1,000/mm3 and/or platelet count < 100,000/mm3. CR and CRi were confirmed just prior to allogeneic HSCT in bone marrow and peripheral blood. Cytogenetic risk group was assigned based on CIBMTR criteria. Chemotherapy regimens prior to allogeneic HSCT defined as follows; standard-dose (cytarabine plus anthracycline), high-dose (cytarabine at individual dose ≥ 1g/m2 with or without other drugs), low-dose (azacitidine or low dose cytarabine). Categorical and continuous variables were analyzed using Fisher's exact test and Mann-Whitney U test, respectively. Overall survival (OS) and relapse free survival (RFS) were estimated by Kaplan-Meiyer method. Cumulative incidence of relapse (CIR), non-relapse mortality (NRM), engraftment rate and cumulative infectious events were calculated using Grayfs method. Multivariate analysis was performed using the Fine-gray proportional hazard regression model for NRM and cumulative infectious events.
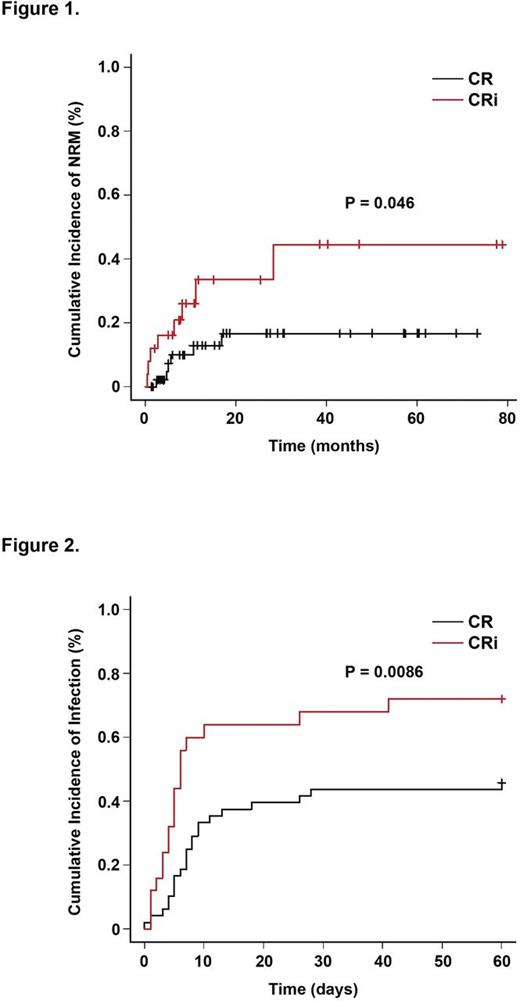
Results: A total of 48 (66%) were in CR and 25 (34%) in CRi. The characteristics of the study population, donors and transplants stratified by blood count recovery pre-HSCT are summarized in Table 1. There were several statistically differences between patients in CR and CRi. More patients in CR had longer time from final chemotherapy to HSCT, lower HCT-CI and a higher proportion of major ABO mismatch donor. Median follow-up from allogeneic HSCT was 18 months (range, 1 to 80 months) in the patients still alive. Patients in CR and CRi had a similar 2-year OS (63% vs. 60%, p = 0.29), 2-year RFS (58% vs. 54%, p = 0.42) and 2-year CIR (30% vs. 19%, p = 0.64). 2-year NRM was significantly higher for patients in CRi (17% vs. 34%, p = 0.046) (Figure 1). Ten patients in CRi (40%) died after allogeneic HSCT. One patient died from relapse of AML. Causes of NRM were infection (n=2), veno-occlusive disease (n=3), respiratory failure (n=3) and chronic graft-versus-host disease (n=1). The median time of neutrophil engraftment was 15 days for patients in CR (range, 10 to 25 days) and 18 days for patients in CRi (range, 11 to 49 days). Engraftment rate of neutrophil for patients in CR and CRi was 96% and 92%, respectively. 2 patients in CRi died before neutrophil engraftment. Engraftment rate of neutrophil within 30 days after allogeneic HSCT was significantly lower for patients in CRi (96% vs 84%, p = 0.037). The median time of platelet engraftment was 22 days for patients in CR (range, 10 to 77 days) and 26 days for patients in CRi (range, 12 to 164 days). Engraftment rate of platelet for patients in CR and CRi was 92% and 80%, respectively. 3 patients in CRi died before platelet engraftment. Engraftment rate of platelet within 60 days after allogeneic HSCT was lower for patients in CRi (85% vs. 65%, p = 0.093). To assess the effect of delayed engraftment, we examined infectious events, including bacteria, fungus and virus, within 60 days after allogeneic HSCT. Significantly more patients in CRi had higher cumulative infectious events (46% vs. 72%, p = 0.0086) (Figure 2). There was no bleeding event within 60 days after allogeneic HSCT. Multivariate analysis demonstrated that CRi was an independent risk factor of early infection after allogeneic HSCT (hazard ratio: HR 2.65, 95% CI: 1.37-5.08, p = 0.0037) without a difference in NRM (HR 1.21, 95% CI: 0.26-5.59, p = 0.81).
Conclusion: Our data, although retrospectively collected, show that incomplete blood count prior to allogeneic HSCT is a predictable marker of early infection after HSCT in patients with AML. This suggests that we need to develop prophylactic strategies for early infection after allogeneic HSCT based on risk assessments.
Maeda:Mundipharma KK: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal