Abstract
Background: The clinical course in CLL is very heterogeneous ranging from stable disease to a rather rapid progression requiring treatment. The acquisition of genetic abnormalities termed clonal evolution (CE) is likely to correlate with clinical progression and might be used to guide treatment strategies.
Aim: The aim of this study was to evaluate the frequency of CE on the cytogenetic (CCE) and molecular genetic (MCE) levels and its association with the IGHV mutation status and clinical outcome.
Methods: 179 CLL cases were selected on the basis that chromosome banding analysis (CBA) and mutation analyses in TP53 and SF3B1 all having been performed at least at two time points. The median age at first evaluation was 72 years (range: 46-95). The first time point of analysis was at primary diagnosis (n=131) or during course of disease but prior to any treatment (n=48). In all patients interphase FISH was performed with probes for 17p13 (TP53), 13q14 (D13S25, D13S319, DLEU), 11q22 (ATM), and the centromeric region of chromosome 12 and the IGHV mutation status was evaluated. A total of 465 CBA, 417 TP53 and 424 SF3B1 mutation analyses were evaluated. The median number of samples per patient was 2 (range: 2-9). The time between samples ranged from 1 month to 9.8 years (median 21 months). For all patients clinical follow-up data was available with a median follow-up of 7.4 years and 5-year overall survival (OS) of 88%.
Results: At first investigation CBA revealed a normal karyotype in 31 (17%) patients. In cases with an aberrant karyotype the pattern of abnormalities was typical for CLL: del(13q); 51% (homozygous: 15%), +12: 18%, del(11q): 16%, and del(17p): 5%. A complex karyotype (≥3 abnormalities) was present in 18%. The IGHV status was unmutated (IGHV-U) in 56% of cases and TP53 and SF3B1 mutations were detected in 10% and 15%, respectively.
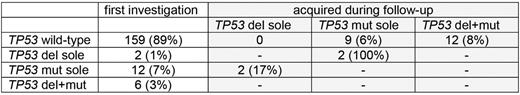
CCE was observed in 63/179 patients (35%). The median time to CCE was 46 months (range 3-111). The most frequent abnormalities gained during CCE were loss of 17p (14/63; 22%), 13q (11/63; 18%), and 11q (10/63; 16%). Acquired loss of 17p was more frequent in SF3B1mutated CLL (19% vs 6%, p=0.04). MCE was observed in 29/179 cases (16%). TP53 and SF3B1 mutations were acquired during the course of the disease in 23 (14%) and 7 (5%) cases, respectively. The median time to MCE was 61 months (range 1.5-109). Of note, in 2 cases with TP53 deletion a TP53 mutation was acquired and in 2 cases with TP53 mutation a TP53 deletion was acquired. In 12 CLL both a TP53 deletion and a TP53 mutation were acquired (table).
CCE and MCE were significantly associated with IGHV-U (p=0.003; p<0.001) and with each other (p<0.001). In more detail, in 71% of cases with CCE and 90% of cases with MCE an IGHV-U was present. Thus, CCE and MCE were less frequent in IGHVmut CLL (23% and 4%). In 30% of CLL with CCE also MCE occurred. In addition CCE was associated with an aberrant karyotype at first investigation (p<0.001). CCE occurred in only 3% of CLL with a normal karyotype but in 42% of CLL with an aberrant karyotype.
Time to treatment was significantly shorter in patients with CCE, MCE and both compared to the respective patients without (2.1 vs 5.5 yrs, p=0.004; 1.8 vs 4.8 yrs, p=0.07; 2.2 vs 5.3 yrs; p=0.04). While no impact of CCE on OS was observed in patients with a mutated IGHV status, in patients with an unmutated IGHV status a tendency to shorter OS was observed in cases with CCE compared to those without (7 year OS: 67% vs 83%; p=0.2). No impact on OS was observed for MCE. This may be due to rather short follow up after CE. However, if CCE and MCE resulted in CLL harboring both TP53 deletion and TP53 mutation 5 year OS was significantly shorter than in CLL with neither TP53 deletion nor TP53 mutation (75% vs 91%, p=0.03).
Conclusions: 1) We observed CCE in 35% and MCE in 16% of CLL. 2) The pattern of cytogenetic abnormalities acquired during the course of the disease is similar to the pattern observed in CLL at diagnosis, however the frequency varies with del(17p) being the most frequently gained in CE. 3) CCE and MCE were highly correlated to IGHV-U. 4) In 25% of CLL with CCE and MCE CE resulted in the co-occurrence of TP53 deletion and TP53 mutation, which was associated with a significantly shorter OS emphasizing the necessity to reevaluate the TP53 status during the course of the disease to guide treatment. 5) The frequency and impact of CE needs to be further studied in unselected patient cohorts in which CBA and mutational analysis is performed on a regular basis.
Haferlach:MLL Munich Leukemia Laboratory: Employment, Equity Ownership. Jeromin:MLL Munich Leukemia Laboratory: Employment. Nadarajah:MLL Munich Leukemia Laboratory: Employment. Zenger:MLL Munich Leukemia Laboratory: Employment. Kern:MLL Munich Leukemia Laboratory: Employment, Equity Ownership. Haferlach:MLL Munich Leukemia Laboratory: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal