Abstract

Background:
Based on a model suggesting leukemia can be driven by combined effect of mutations in an epigenetic gene (DNMT3) and Ras, the combination of a hypomethylating agent (HMA) such as azacitidine (AZA) and a Ras mimetic such as rigosertib (RIG) may have enhanced activity in both MDS and AML. The mechanism of action for RIG (Athuluri-Divakar et al, Cell 2016) documents its interference with the RAS-binding domains of RAF kinases and inhibition of the RAS-RAF-MEK and the PI3Ks pathways. In vitro, the combination of RIG with AZA was found to act synergistically to inhibit growth and to induce apoptosis of leukemic cells in a sequence-dependent manner (exposure to RIG first, followed by AZA) (Skidan et al, AACR 2006). Rigosertib's low bone marrow toxicity in pre-clinical assays, effective inhibition of human hematopoietic tumor cell lines, and its synergy with AZA suggests the potential value of combination treatment for patients (pts) with MDS.
Phase I results of the current clinical study in pts with MDS or AML showed the combination of oral RIG and standard-dose AZA to be well-tolerated with evidence of efficacy (Navada et al, Blood 2014). The phase II portion of the study was initiated to further evaluate the combination in pts with MDS.
Methods:
Phase II results are presented for HMA-treatment-naïve MDS pts and for those with MDS failing to respond to or progressed on a prior HMA. Oral RIG was administered twice daily on Day 1-21 of a 28-day cycle at the recommended Phase II dose (RPTD: 560 mg qAM and 280 mg qPM). AZA 75 mg/m2/d SC or IV was administered for 7 days starting on Day 8. A CBC was performed weekly and a bone marrow aspirate and/or biopsy were performed at baseline, D29, and then every 8 weeks thereafter.
Results:
The combination of oral RIG and injectable AZA has been administered to a total of 54 pts, of whom 40 were pts with MDS including HMA-treatment-naïve (N=23) and previously HMA treated pts (N=17). Median age was 66 years (range 25-85); 73% of pts were male; and ECOG performance status was 0, 1, and 2 in 23%, 73%, and 5%, respectively. 17 pts received prior HMA therapy: 12 AZA, 4 decitabine, and 1 both. Patients have received 1-36+ cycles of treatment (median, 6 cycles), with a median duration of treatment of 25 weeks (range 4 to 145+ weeks). 8 (20%) and 2 (5%) of pts have been treated for more than 1 and 2 years, respectively.
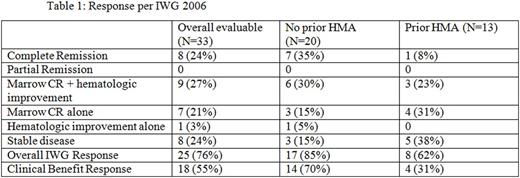
Table 1 shows the response per IWG 2006 criteria (Cheson, Blood 2006) among 33 evaluable patients. The response per IWG 2006 was complete remission (CR) in 8 (24%), concurrent marrow CR and hematologic improvement (HI) in 9 (27%), marrow CR alone in 7 (21%), and HI alone in 1 (3%). When overall response is defined as CR plus PR plus HI - responses with improvement in marrow function and thus either normalization of the peripheral blood count or lineage improvement - defined here as Clinical Benefit Response - 55% of all evaluable pts and 70% of the evaluable HMA-treatment-naïve patients showed responses meeting these criteria.
Median time to initial response was 2 cycles (2.2 months), and median time to best response was 3 cycles (3.3 months). Median duration of response was 8 months for CR, 14.3 months for marrow CR, 7.4 months for erythroid response, 8 months for platelet response, and 6.2 months for neutrophil response.
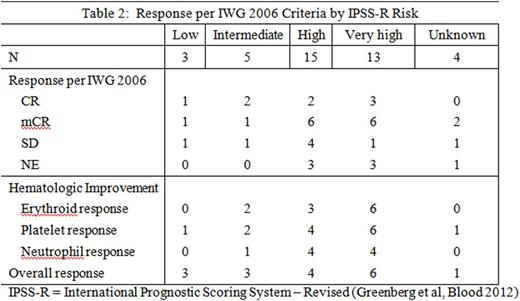
Clinical response is classified by IPSS-R risk categories below.
The most frequently reported adverse events are nausea (41%), fatigue (39%), diarrhoea (37%), constipation (37%), dysuria (28%), decreased appetite (28%), haematuria (24%, 8% Grade 3), pyrexia (24%), dizziness (22%), thrombocytopenia (20%), back pain (20%), dyspnoea (20%), and cough (20%).
Eight deaths were reported on study with most common causes including infection and progression of disease.
Conclusions:
The combination oforalRIG and standard-dose AZA was well tolerated in repetitive cycles in pts with MDS. Response per IWG 2006 criteria was observed both in HMA-treatment-naïve patients (85%) and in patients after failure of prior HMA therapy (62%); employing Clinical Benefit Response as the criteria, these groups had 70% and 31% response, respectively. These clinical results confirm the preclinical synergistic interaction with the combination of RIG and AZA reported by Skidan et al, and suggest that the combination can overcome clinical resistance to HMAs. Based on these results, a Phase III study of the combination of oral RIG and AZA in patients with MDS is planned.
Navada:Onconova Therapeutics, Inc.: Research Funding. Daver:Karyopharm: Honoraria, Research Funding; Pfizer: Consultancy, Research Funding; Sunesis: Consultancy, Research Funding; Ariad: Research Funding; Otsuka: Consultancy, Honoraria; Kiromic: Research Funding; BMS: Research Funding. DiNardo:Agios: Other: advisory board, Research Funding; Novartis: Other: advisory board, Research Funding; Celgene: Research Funding; Abbvie: Research Funding; Daiichi Sankyo: Other: advisory board, Research Funding. Konopleva:Reata Pharmaceuticals: Equity Ownership; Abbvie: Consultancy, Research Funding; Genentech: Consultancy, Research Funding; Stemline: Consultancy, Research Funding; Eli Lilly: Research Funding; Cellectis: Research Funding; Calithera: Research Funding. Fenaux:Celgene, Janssen,Novartis, Astex, Teva: Honoraria, Research Funding. Petrone:Onconova Therapeutics, Inc.: Employment. Zbyszewski:Onconova Therapeutics, Inc.: Employment. Fruchtman:Onconova: Employment. Silverman:Onconova Therapeutics, Inc.: Patents & Royalties: Co-Patent holder for the combination of azacitidine and rigosertib, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal