Abstract
Introduction: BCR-ABL kinase domain (KD) mutations have well established role in tyrosine kinase inhibitors (TKIs) resistance and disease progression in chronic myeloid leukemia (CML)1. In recent years, compound BCR-ABL mutations have emerged as a new threat to CML patients by causing higher degrees of resistance involving multiple TKIs, including ponatinib2. However, there are limited reports about association of compound BCR-ABL mutations with disease progression in imatinib sensitive CML patients3. Furthermore, BCR-ABL mutation detection is currently recommended only in case of drug resistance and disease progression and clinical significance of BCR-ABL mutation detection in TKI responder chronic phase CML is not well documented4. Therefore, we investigated presence of ABL-KD mutations in chronic phase (CP) and advanced phase imatinib sensitive CML to find out association of BCR-ABL mutations with progression to advanced disease phases in CML patients. .
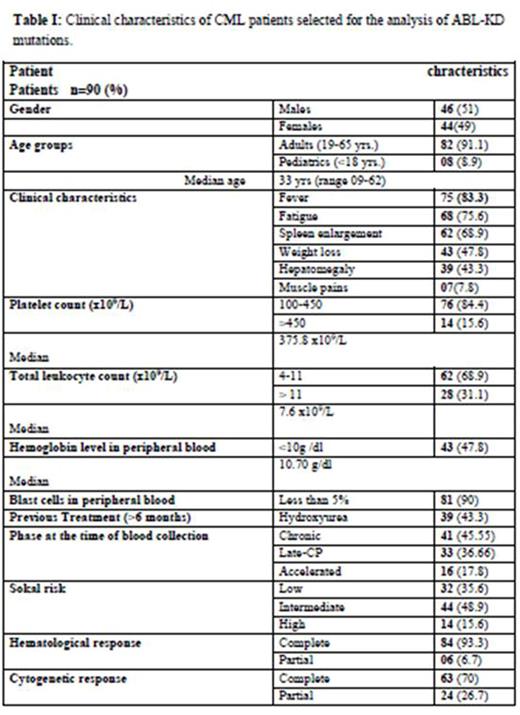
Patients and Methods: Imatinib sensitive CML patients in CP and advanced phases of the disease were included in the study.All CP patients were incomplete hematological, complete cytogenetic and major molecular responses. Due to specific study objectives, patients manifesting drug resistance during follow-up studies were excluded from the study. A total of 90 imatinib sensitive CML patients (CP=41, late CP=33, and accelerated phase=16) were finally available for analysis. All patients as well as 10 healthy controls were investigated for BCR-ABL mutations using Sanger sequencing. All response criteria were per European LeukemiaNet guidelines4. Data was analyzed using SPSS software (version 19).
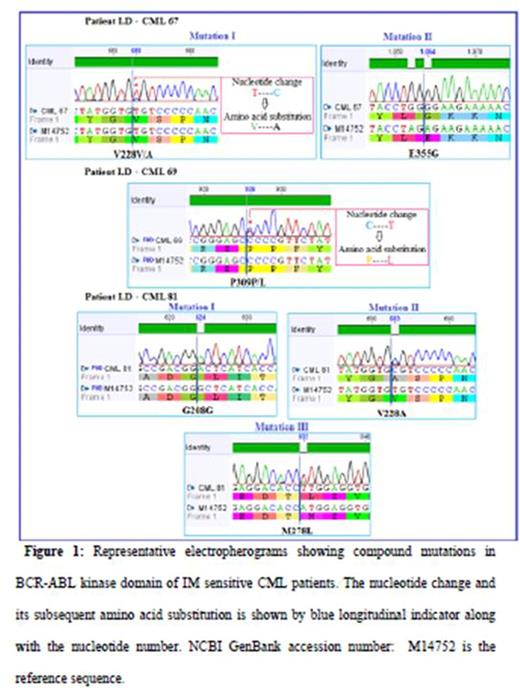
Results: Mean age of the patients was 33 years (Table 1). Eleven out of 33 (33.3%) patients in late-CP CML harbored 24 types of point mutations, out of which eight (72.72%) harbored compound mutated sites (Figure 1, Table 2). E355G (3.33%) was the most prevalent mutant. Five patients (45.45%), all of which had compound mutations, progressed to advanced phases of disease during follow up studies. No BCR-ABL mutation was detected in healthy subjects and in early CP CML patients. Therefore, early CP CML patients served as additional control in this study. BCR-ABL mutations were found in 3 accelerated phase patients as well. Late-CP mutations were associated with elevated platelet count (p= 0.037) and male gender (p= 0.049). The median overall survival and event free survival of CML patients (n=90) was 6.98 and 5.8 years respectively. Seven year survival was found to be 94.2%.
Discussion and conclusions: Compound BCR-ABL mutations were associated with progression to advanced disease in imatinib sensitive late-CP CML patients. Although single BCR-ABL mutations have previously been found to cause CML progression5, this is first report of association of compound BCR-ABL mutations with disease progression in stable imatinib responders at late CP. Detection of new mutations can help in defining mechanism of CML progression6. Moreover, BCR-ABL mutation detection in late CP CML patients sensitive to TKI treatment can help in early assessment of risk for disease progression and/or drug resistance and subsequent clinical intervention to delay disease progression which is a major challenge of CML therapy in TKI era7.
References:
1. Haznedaroglu IC. Mediterranean journal of hematology and infectious diseases 2015;7.
2. Khorashad JS, Kelley TW, Szankasi P, Mason CC, Soverini S, Adrian LT, Eide CA, Zabriskie MS, Lange T, Estrada JC. Blood 2013;121:489-98.
3. Deininger MW, Hodgson JG, Shah NP, Cortes JE, Kim DW, Nicolini FE, Talpaz M,Baccarani M, Müller MC, Li J, Parker WT, Lustgarten S, Clackson T, Haluska FG,Guilhot F, Kantarjian HM, Soverini S, Hochhaus A, Hughes TP, Rivera VM, Branford S. Blood. 2016 Feb 11;127(6):703-12.dddd
4. 7. Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF, Cervantes F, Clark RE, Cortes JE, Guilhot F. Blood 2013;122:872-84.
5. Carella AM, Garuti A, Cirmena G, Catania G, Rocco I, Palermo C, Pica G, Pierri I, Miglino M, Ballestrero A, Gobbi M, Patrone F. Leukemia & lymphoma 2010;51:275-8.
6. Giotopoulos G, van der Weyden L, Osaki H, Rust AG, Gallipoli P, Meduri E,Horton SJ, Chan WI, Foster D, Prinjha RK, Pimanda JE, Tenen DG, Vassiliou GS,Koschmieder S, Adams DJ, Huntly BJ. J Exp Med. 2015 Sep 21;212(10):1551-69.
7. Mukherjee S, Kalaycio M. Curr Hematol Malig Rep. 2016 Apr;11(2):86-93.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal