Abstract
Introduction: Mantle cell lymphoma (MCL) is a B-cell neoplasm that has a characteristic immunophenotype of being positive for CD5, B-cell antigens and cyclin D1. A small subset of cases of MCL can be negative for CD5, approximately 5% in the literature. The clinicopathologic features and prognosis of patients with CD5-negative MCL are poorly characterized. Here, we study a group of patients with CD5- MCL and compare them with a group patients with CD5+ MCL.
Methods: From a total of 270 cases of MCL accessioned from 2004-2015, 58 CD5- cases (study group) and 212 CD5+ cases (control group) were identified. All cases of MCL were positive for cyclin D1 by immunohistochemistry and, in most patients, CCND1-IGH was shown FISH. Cases negative for CD5 were assessed by flow cytometry and/or immunohistochemistry. Fisher exact test was utilized to analyze differences between the CD5- and CD5+ groups. Patient survival was analyzed using the Kaplan-Meier method and compared using the log-rank test. Univariate and multivariate Cox proportional hazards model analyses for OS and PFS were performed (SPSS 22 software). A P-value of less than 0.05 was considered statistically significant.
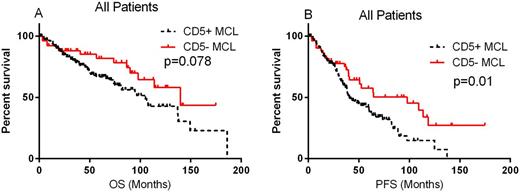
Results: The CD5- group included 39 men and 19 women with a median age of 66 years (range, 36- 88 years) at time of diagnosis. The CD5- and CD5+ groups shared overlapping clinicopathological features, but CD5- cases showed a lower percentage of men (P=0.006) than CD5+ cases. Treatment information was available for 50 patients. Twenty-nine (58%) patients were treated initially with R-Hyper CVAD therapy (rituximab, fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone alternating with high dose methotrexate and cytarabine). Seventeen (34%) patients were treated initially with less aggressive therapy: 7 with R-CHOP; 8 had other rituximab-based chemotherapy regimens; 2 received rituximab as a single agent. Four patients (8%) were observed without therapy. After induction, 34 patients achieved complete remission (CR), 5 patients achieved partial remission (PR), 6 patients showed no response (NR) or progressive disease (PD), and 5 patients lost follow-up. Ten patients also underwent stem cell transplantation (SCT): 5 patients received allogeneic SCT, the other 5 autologous SCT. With a median follow-up of 45.7 months (range, 2.0-174.3 months), 13 of 56 (23.2%) patients died, 43 of 56 (76.8%) patients were alive at last follow-up, and the rest of 2 patients lost follow up. The induction chemotherapy regimens and CR and PR rate were not significantly different between the CD5- and CD5+ groups (p>0.05). Survival analysis showed patients with CD5- MCL had a tendency for longer OS (Figure 1A, P=0.078). Further analysis showed that lack of CD5 expression predicted a superior OS in a few subsets of MCL patients defined with 1) normal WBC count (p=0.049); 2) Stage I/II disease (p=0.046); 3) Low/intermediate MIPI (p=0.041) and 4) Ki67≥30% (at a borderline p value of 0.05). Patients with CD5- MCL also showed a significantly longer progression-free survival (PFS) (Figure 1B, P=0.01). Absence of CD5 expression was associated with a better PFS in MCL patients with advanced disease (stage III-IV) (P=0.035), a normal leukocyte count (P=0.018), a normal serum lactate dehydrogenase level (P=0.046), classical morphology (P=0.029), and low/intermediate MIPI (p=0.0004). Multivariate Cox regression analysis revealed that MIPI was the only independent prognostic factor for both OS and PFS (P=0.026 and P=0.001 respectively) and CR/PR also predict a better OS (P=0.004) in CD5- MCL patients.
Conclusion: The clinicopathologic features were similar between patients with CD5- MCL and those with CD5+ MCL, except that less men in the CD5- MCL group. Lack of CD5 expression was associated with a favorable PFS in MCL patients. Recognizing this subgroup of CD5- MCL has not only a diagnostic significance, but also a prognostic significance.
Wang:Acerta Pharma: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Juno Therapeutics: Research Funding; Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Kite Pharma: Research Funding; Asana BioSciences: Research Funding; BeiGene: Research Funding; Pharmacyclics: Research Funding; Celgene: Research Funding; Onyx: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal