Abstract
The range of genomic drivers of leukemogenesis and clonal nature of the disease illustrate the heterogeneity of the mutational spectrum in AML. Genomic interrogation of the evolution of AML has begun to highlight the scope of somatic changes that occur between diagnosis and relapse. A total of 1,214 patients were treated on the Children's Oncology Group trials AAML03P1 and AAML0531, of which 398 had relapse after initial remission. Of this cohort, 201 patients had matching diagnostic and relapse specimens for molecular profiling for the most common somatic mutations in pediatric AML (FLT3/ITD, FLT3/ALM, NPM1, CEBPA, WT1, NRAS, and KIT). Sequencing techniques included PCR with Sanger sequencing for detection of point mutations and indels and fragment length analysis for FLT3/ITD.
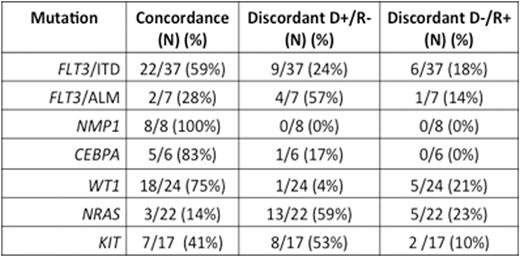
In the cohort, FLT3/ITD was detected in 31/201 (15%) cases at diagnosis. Of the cases with diagnostic ITD, 22 (71%) relapsed with FLT3/ITD. Conversely, of the 28 cases with FLT3/ITD detected at relapse, 6 (21%) did not have detectable ITD at diagnosis. Overall, there were 37 patients (18%) with FLT3/ITD mutations detected at either time point. Of the 37 patients, 22 (59%) demonstrated stability of the mutation from diagnosis to relapse. Discordant mutation status was observed in 15 patients (41%). Among the discordant patients, 9 had FLT3/ITD detected at diagnosis only. Conversely, 6 patients were ITD-positive at relapse only, demonstrating disease evolution with continued mutational acquisition (Table 1). In every discordant case, ultra sensitive PCR analysis confirmed absence of an ITD. The median ITD allelic ratio (AR) for patients with concordant status was 0.47 (range 0.03-2.67) vs. 0.24 (range 0.04-0.47) for those with disappearance of the ITD at relapse, suggesting an association of diagnostic AR with mutation stability.
NPM1 mutations were detected in 8 patients at diagnosis and 100% concordance was observed in the cohort. CEBPA mutations were detected in 6 patients at diagnosis, and in 5 cases remained at relapse. One patient had a CEBPA mutation detected at diagnosis only. FLT3/ALM mutations were detected in 7 patients at either time point. Seven patients had an ALM at diagnosis, however concordance was observed in 2 cases, whereas 4 patients had detection at diagnosis only.
There were 22 patients (11%) with NRAS mutations detected at either time point. Diagnostic NRAS mutations were detected in 18 patients, while only 3 (17%) had the identical mutation detected at relapse, as one patient had a distinct mutational sequence present at relapse. NRAS mutations were detected at diagnosis only in 13 patients (59%), where as 5 patients (23%) had a mutation detected at relapse only. NRAS was the most discordant mutations analyzed, with only 3/22 patients (14%) demonstrating stability of the mutation from diagnosis to relapse (Table 1).
WT1 exon 17 indels were observed in 24 patients (12%) at either time point. Nineteen patients had diagnostic mutations, with 18 patients demonstrating stability at relapse. Five patients had mutations detected at relapse only. Overall, concordance was observed in 18 patients (75%). Only 1 alteration was detected at diagnosis in all patients, however 6 patients with concordant WT1 status had multiple indels detected at relapse, demonstrating continued mutational acquisition. KIT mutations (missense and indels) in exons 8 (n=11) and 17 (n=7) were detected in 17 patients. Mutational concordance was observed in 7 patients. Eight patients had mutations detected at diagnosis only, while 2 patients had mutations detected at relapse only (Table 1).
We demonstrate the complexity of the evolving somatic landscape from diagnosis to relapse in pediatric AML. The stability of NPM1 mutations, considered an early leukemogenic event, is in contrast to the discordant NRAS and KIT mutations. There was evolution of FLT3/ITD status, and we observed overall higher ARs in the concordant cohort, perhaps suggesting mutations in this cohort served as stronger leukemic drivers. Further investigation on the biologic implications and clonal prevalence is critical to determine a mutation's significance in leukemogenesis, timing of acquisition, and if appropriate for therapeutic targeting and disease monitoring.
Mutational concordance from diagnosis to relapse.
Legend:
Discordant D+/R-: Discordant status with diagnostic only positive
Discordant D-/R+: Discordant status with relapse only positive
Mutational concordance from diagnosis to relapse.
Legend:
Discordant D+/R-: Discordant status with diagnostic only positive
Discordant D-/R+: Discordant status with relapse only positive
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal