Abstract
Activation of MAPK signaling is characteristic of many cancers, and approximately 15% of AML patients carry activating RAS mutations. The PI3K pathway is also constitutively activated in AML. Both pathways interact with each other extensively and provide compensatory signaling when one pathway is inhibited. It has been demonstrated in vitro that concurrent inhibition of both pathways is effective in blocking the proliferation of AML cell lines through an immediate decrease in pAkt and pErk, leading to inhibition of pS6 (Gritsman et al, J Clin Invest, 2014, 124(4):1794-1809). The combination of alpelisib (BYL-719), which inhibits PI3K (p110alpha), and binimetinib (MEK-162), which inhibits MEK (MAPK pathway), was tested in various tumor types in the Phase Ib Clinical Trial CMEK162x2109. We present here the clinical data and correlative phosphoprotein analysis of 6 patients with relapsed refractory RAS-mutated AML treated at Massachusetts General Hospital on Extension Arm 4A of this trial.
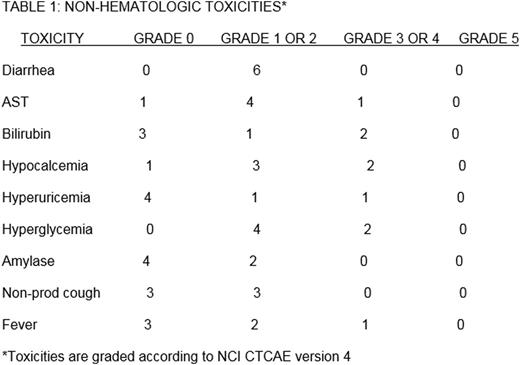
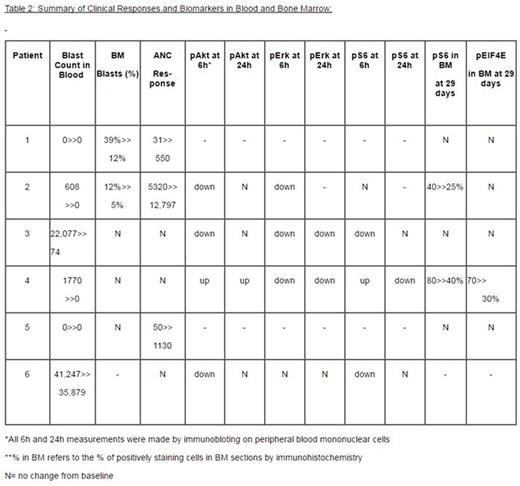
Entry to this trial was restricted to adult patients with RAS-mutated AML previously treated with 1 or 2 prior chemotherapy regimens or for whom there was no known effective therapy. Patients received 200mg QD of alpelisib and 45mg BID of binimetinib concurrently and continuously with adjustments for toxicities. Hematologic toxicity could not be determined in these patients with active AML causing myelosuppression. There were responses in blood and/or bone marrow (BM) in 3 patients, but none made partial response criteria by IWG guidelines, mainly due to platelet counts <100,000/ul. Blast clearance from blood in the first month were seen in 2 patients, with a >50% reduction in a third patient. A rise in absolute neutrophil count was seen in 3 patients, 2 from below 100/ul to above 500/ul, and in 1 from 5,320/ul to 12,797/ul during the first month. BM partial responses were seen in 2 patients, with blast percentages dropping from 39% to 10% in 1 patient and from 12% to 5% in another.
We analyzed the effects of this drug combination on signaling targets by collecting peripheral blood samples on day 1 pre-treatment and at 6 and 24 hours post-initiation of treatment. In 4 patients, we performed analysis of the phosphorylation of Akt, ribosomal protein S6, Erk, STAT5, and STAT3 on timed peripheral blood samples by immunoblotting. In all 4 cases at baseline, pAkt, pErk, and pS6 were detectable, while pSTAT5 and pSTAT3 levels were variable. In 3 of 4 cases, we observed a transient decrease in pAkt at 6 hours, but then a rebound at 24 hours. In 3 of 4 cases, we observed a lack of sustained pS6 inhibition. We observed sustained pErk inhibition at 24 hours in 2 cases. One patient who had blood blast clearance, improvement in ANC, and a drop in bone marrow blasts, showed strong inhibition of pAkt and pERK at 6 hours, although pS6 did not decrease. In another case we performed phospho-flow cytometry on timed whole blood samples. We observed an increase in pAkt, pS6, and pErk from baseline at 24 hours, both in CD34+38+blasts, and in the primitive CD34+38- cells. This second patient showed no clinical benefit from the treatment in terms of blood blast count, ANC, or platelets.
We also performed immunohistochemistry for pS6, pErk, pAkt, pSTAT5, pSTAT3, p-eIF4E, and Caspase 3 on BM sections obtained at diagnosis and at one month and two months post-initiation of treatment, when available. These studies generally showed either persistence or an increase in the pS6 and p-eIF4E signals, both indicators of mTORC1 activity, in post-treatment BM samples. Levels of pAkt, pErk, pSTAT5 and pSTAT3 were highly variable in the post-treatment bone marrow samples.
In conclusion, we demonstrated some initial target inhibition with the concurrent use of alpelisib and binimetinib in a subset of patients. However, inhibition of late downstream targets was not sufficiently sustained to achieve consistent clinical benefit in our patients with RAS-mutated AML. While the strategy of concurrent inhibition of various critical signaling pathways remains interesting, sustained inhibition of downstream signaling may require a different dosing schedule of the two drugs. Given the incomplete inhibition of mTORC1 targets pS6 and p-eIF4E in most cases, the addition of a third agent to inhibit pathways causing cross-activation downstream of mTORC1 may be required.
Weinstock:Novartis: Consultancy, Research Funding. Fathi:Bexalata: Other: Advisory Board participation; Merck: Other: Advisory Board participation; Celgene: Consultancy, Research Funding; Seattle Genetics: Consultancy, Other: Advisory Board participation, Research Funding; Agios Pharmaceuticals: Other: Advisory Board participation.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal