Abstract

Background
Hydroxyurea (HU), a chemotherapeutic agent and an approved therapy for sickle cell disease (SCD), increases cGMP levels and thereby increases fetal hemoglobin (HbF) levels in RBC, which generally correlates with decreased hemolysis and reduced disease severity in subjects with SCD. In addition, increased cGMP levels are anti-inflammatory and reduce the adhesion of WBC to the vascular endothelium. However, potential adverse effects of HU such as infertility, susceptibility to infections, or teratogenic effect have been the subject of concerns. Phosphodiesterase-9 inhibitors (PDE9i) may provide an alternative to HU because of their ability to inhibit the degradation of cGMP and increase cellular cGMP levels. Previously described PDE9i were developed to inhibit neuronal PDE9 for neurologic diseases, like Alzheimer's. A PDE9i with low brain penetrance may be preferable for the chronic treatment of SCD adults and children. IMR-687 is a safe, potent, PDE9i being developed specifically for SCD without these liabilities of HU or the high brain penetrance of other PDE9is.
Hypothesis
We hypothesized that PDE9i's will increase cellular cGMP levels in hematopoietic cells, increase HbF in red blood cells (RBC), inhibit RBC sickling, decrease inflammation (leukocytosis), and inhibit vaso-occlusion in murine models of SCD.
Results & Methods
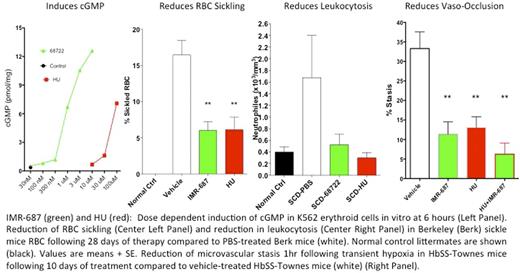
IMR-687, is a potent inhibitor of PDE9A (IC50 <10 nM) and demonstrates >100-fold higher IC50 with other phosphodiesterases. To determine the ability of IMR-687 to induce cGMP, K562 erythroid cells were exposed to increasing concentrations of IMR-687 or HU and cGMP assessed at 6 hours. IMR-687, at much lower drug concentrations, induced higher levels of cGMP than HU at 6 hours (Fig. Left Panel).
We next tested IMR-687 in the Berkeley (Berk) mouse model of SCD. Groups of 7-8 Berk SCD mice were dosed by gavage with either vehicle, 30 mg/kg/day of IMR-687, or 100 mg/kg/day of HU. After 30 days of treatment, both IMR-687 and HU resulted in statistically significant decreases in the percentage of sickled RBCs (Fig. Center Left Panel) and increases in the percentage of HbF positive RBCs relative to controls. In addition, both compounds led to statistically significant decreases in total bilirubin, spleen weight and total leucocyte counts (Fig. Center Right Panel).
The ability of IMR-687 to reduce microvascular stasis (% non-flowing venules) was assessed in HbSS-Townes transgenic sickle mice after transient hypoxia and re-oxygenation. Groups of 3 mice/group were dosed orally via drinking water with IMR-687 (30 mg/kg/day), HU (100 mg/kg/day) or vehicle for 10 days. After 10 days of treatment, the mice were exposed to transient hypoxia. Compared with controls, 30 mg/kg/day IMR-687 and 100 mg/kg HU produced statistically significant reductions in microvascular stasis at both 1-hour (Fig. Center Right Panel) and 4-hour time points post-hypoxia. In addition, IMR-687 significantly reduced the proportion of sickled RBCs, increased the number of HbF positive red cells, and reduced the white count.
Lastly, low brain penetration of IMR-687 was confirmed after IV dosing in the rat, with brain concentrations >20 times lower than those in the plasma at all time points assessed. Consistent with this, treatment of C57Bl/6J mice with 10 mg/kg/day IMR-687 for 5 days displayed no effect on locomotor activity or classical fear conditioning (an animal model of learning and memory). In contrast, treatment with a brain penetrant PDE9i, developed for the treatment of neurologic diseases, significantly increased conditioned fear responses in these mice.
Conclusions
IMR-687 increases HbF levels, and reduces red cell sickling, leukocytosis and microvascular stasis, without the observed toxicities of HU. IMR-687 may offer a once a day, oral, safe replacement for HU in the treatment of SCD.
McArthur:Imara: Equity Ownership, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties: Patent; Cydan Development: Employment, Equity Ownership. Maciel:Imara: Research Funding. Chen:Imara: Research Funding. Fricot:Imara: Research Funding. Kobayashi:Imara: Equity Ownership; Cydan Development: Employment. Nguyen:Imara: Research Funding. Parachova:Imara: Patents & Royalties. Abdulla:Imara: Research Funding. Vercellotti:Imara: Research Funding. Svenstrup:Imara: Consultancy, Patents & Royalties. Belcher:Imara: Research Funding; CSL-Behring: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal