Abstract
Introduction
Allogeneic stem cell transplantation (allo-SCT) is a curative treatment for several hematological diseases. Donor-recipient histo-incompatibility is associated with poorer outcome. Transplant outcome of CMV positive patients is reported to be poorer, if the unrelated donor is CMV negative (CMV-mismatch). Recent developments in transplant strategies including high resolution HLA-typing, toxicity-reduced conditioning regimens, CMV-monitoring, and improved supportive care have made transplants from HLA- as well as CMV- mismatched unrelated donors more feasible. We present a retrospective registry analysis from a large, and recent cohort of patients transplanted under these conditions.
Patients and methods:
We report data from adult recipients of allo-SCT treated between 2005 and 2013 in 10 transplant centers across Germany. Inclusion criteria were: 1.) consecutive patients from each center with AML or MDS as reported to the German Stem Cell Transplant Registry (DRST), 2) age >/= 18 years, 3) availability of high-resolution typing for HLA-A, -B, C, DRB1 and DQB1 in case of unrelated donor. Patients with ex-vivo T cell depletion were excluded.
3215 patients with AML (n = 2648) or MDS (n = 567) were included in the study. Donors were matched related (MRD, n =872), matched unrelated (MUD, n = 1553) or mismatched unrelated (9/10 MMUD, n= 620; 8/10 MMUD n = 137; <8/10 MMUD n = 33). Remission status at transplant was CR (49%), not in CR (40%) or untreated (11%). The vast majority of patients (96%) received peripheral blood stem cell grafts. Conditioning was reduced intensity (51%) or myeloablative (49%) according to EBMT criteria. ATG (56%) or alemtuzumab (8%) were used for in vivo T cell depletion. Median patient age was 56 (18-79) years. Median donor age was 38 (12-80) years. Median follow-up was 54 months (34-81 months). Primary endpoint was overall survival (OS) at 3 years.
Results:
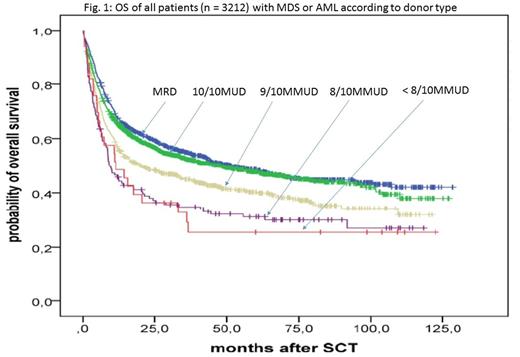
Kaplan-Meier estimates for OS at 3 years was similar after transplants from MRD = 55% (95%CI 51-59%) compared to MUD = 53% (95%CI 51-59%), p = 0.26. OS at 3 years was worse for 9/10 MMUD with 45% (95% CI 41-49%, p<0.001), for 8/10 MMUD with 35% (95% CI: 27%-43%, p < 0.001) and for <8/10 MMUD with 29% (95% CI 13%-45%, p = 0.005) (figure 1).
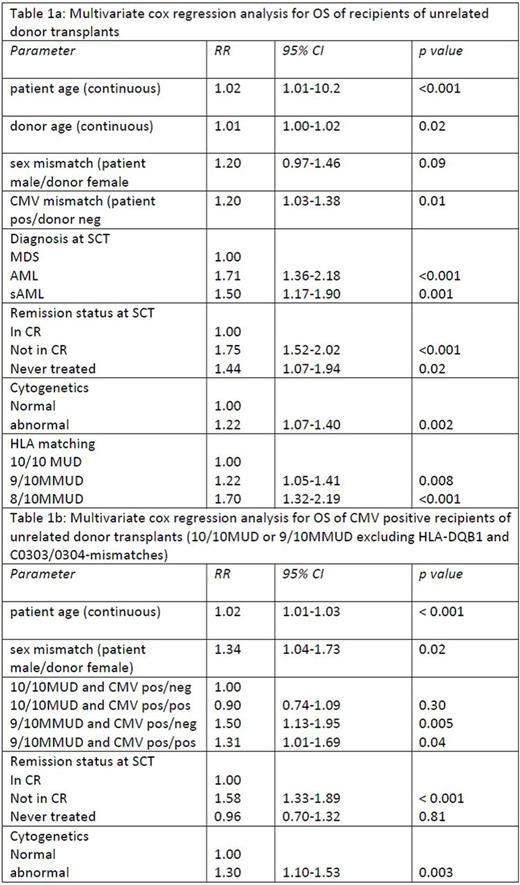
In recipients of unrelated donor transplants, multivariate cox regression analysis revealed significant negative impact of increasing patient age, increasing donor age, sex-mismatch (male patient/female donor), CMV-mismatch (patient pos/ donor neg), diagnosis of AML or sAML compared to MDS, lack of complete remission at transplant, abnormal cytogenetics and HLA-mismatching (table 1a).
In a subgroup analysis restricted to patients transplanted from unrelated donors after myeloablative conditioning and T cell depletion, 3 years OS was better after 10/10 MUD: 60% (55-65%) compared to 9/10 MMUD: 49% (41-57%), p = 0.02. This was also true after reduced intensity conditioning and T cell depletion with ATG, with 3 year OS after 10/10 MUD: 49% (45-53) compared to 9/10 MMUD: 37% (31-43%), p = 0.001. Excluding HLA-DQB1-mismatches and HLA-C0303/0304-mismatches from the 9/10 MMUD group did not significantly alter results.
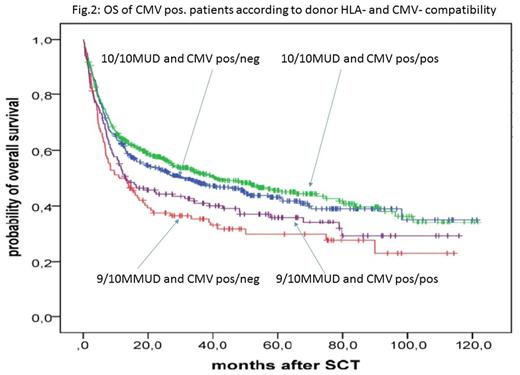
Acknowledging the negative impact of both HLA and CMV-mismatching, we sought to determine which of these two parameters is of higher relevance for donor selection. For this purpose subgroup analyses were performed including only CMV-positive patients who received transplants from an unrelated donor (10/10 MUD or 9/10 MMUD). HLA-DQB1-mismatches and HLA-C0303/0304-mismatches were excluded. For this subgroup of n = 1167 patients multivariate cox regression analysis revealed better outcome after 10/10 MUD from CMV neg. donors compared to 9/10 MMUD from a CMV pos. donors (RR: 1.31, p = 0.04, table 1b and figure 2). Restricting the analysis only to patients who received T cell depletion with ATG did not significantly alter these findings.
Conclusions:
In this large multicenter cohort of recently transplanted patients, we find similar survival outcomes for matched related and fully matched unrelated donor transplants. We confirm the negative impact of HLA-mismatching on survival outcome, irrespective of conditioning intensity. Our results show that though CMV-mismatching is associated with poorer outcome, its relevance is secondary to HLA-mismatching.
Acknowledgments:
This work was supported by a research grant of the DKMS-Stiftung to FA and WB.
Stelljes:Pfizer: Consultancy. Kobbe:Jansen: Honoraria, Other: travel support; Celgene: Honoraria, Other: travel support, Research Funding. Kröger:Sanofi: Honoraria, Research Funding; Neovii: Honoraria, Research Funding; Riemser: Honoraria, Research Funding; Novartis: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal