Abstract
Introduction
While high dose chemotherapy and autologous hematopoietic stem cell transplantation (auto-HCT) is an accepted part of up front therapy for patients with multiple myeloma (MM), the role of this treatment modality for relapsed patients is still evolving. In light of data suggesting safety and synergy in combining novel therapeutics with traditional cytotoxic chemotherapy, we hypothesized that lenalidomide could be safely combined with high dose melphalan in the salvage auto-HCT setting and yield a meaningful duration of disease control.
Methods
We conducted a phase I/II study of lenalidomide and high dose melphalan + auto-HCT. MM patients with relapsed or progressive disease were treated with 7 days of oral lenalidomide (doses of 25, 50, 75 or 100 mg daily for the 7 days) on days (-8) to (-2). High dose melphalan (total of 200 mg/m2) was administered as 100 mg/m2 IV on days (-3) and (-2) followed by auto-HCT on day 0. The Eff-Tox method of Thall, Cook, and Estey was used for dose escalation with cohorts of 3 to maximize the trade-off between efficacy and toxicity, defined as CR at day 90 and regimen-related death, graft failure, or select grade 3+ events within 30 days after transplant, respectively. Kaplan-Meier method was used to estimate progression-free survival (PFS) and overall survival (OS) and the log-rank test was used to assess univariate differences between dose levels. Bayesian logistic regression and survival time models were used for multivariable analyses, with posterior probabilities greater than 0.95 or less than 0.05 considered significant. Initial results after 12.3 months of follow-up were published in 2015; we now present an update with 39.8 months of follow-up.
Results
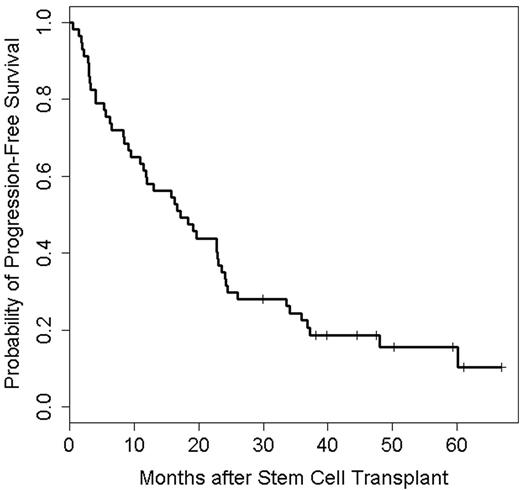
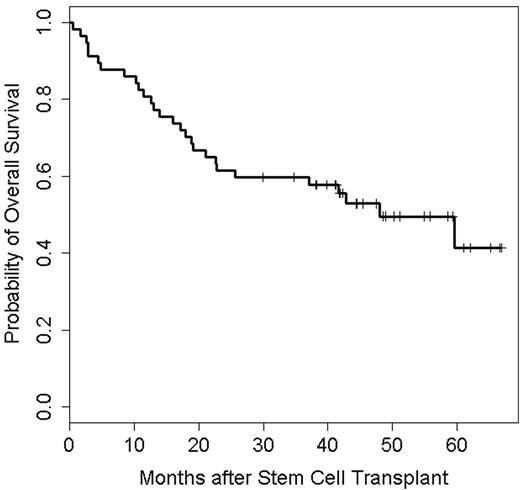
57 patients were enrolled, of which 18 (32%) had received a prior auto-HCT. A total of 3, 5, 24 and 25 patients received 25, 50, 75 and 100 mg of lenalidomide, respectively. Median age at auto-HCT was 60 (34-72) years. Median prior lines of treatment were 3 (1-11). Twenty-two patients (39%) were lenalidomide-refractory at study entry. Patient characteristics did not differ significantly between the lenalidomide dose levels. In total, only 2 dose-limiting toxicities were seen, both at dose level 75 mg. Two patients died of nonrelapse causes (viral infection 1, cardiac failure 1) for a treatment-related mortality of 4%. Median time to both neutrophil and platelet engraftment was 11 days. One patient developed a second primary malignancy (squamous cell cancer of the skin). 63% received maintenance therapy, (54% lenalidomide-based). By day +90, 8 patients (14%) had achieved a complete response (CR), 17 (30%) a very good partial response (VGPR), and 17 (30%) a partial response (PR), with no significant differences in response rates among the 4 lenalidomide dose levels. Best responses were PR: 26%, VGPR: 18%, near CR: 18%, CR: 7%, stringent CR: 23% for a ≥VGPR rate of 66. 23% achieved bone marrow minimal residual disease negativity by flow cytometry. Median time to achieve best response was 92 days (range: 16-732). One patient (2%) had progressive disease and 3 patients (5%) achieved only stable disease. Multivariable Bayesian logistic regression revealed that high-risk cytogenetics, (deletion 13q, t(4:14) or del 17p) by conventional cytogenetics or (t(4:14), t(14:16) or del17p by fluorescent in-situ hybridization), bone marrow disease burden and number of prior lines of treatment were each significantly associated with a lower probability of reaching CR by day 90. With a median follow up of 39.8 months (range: 0.5- 66.9), median PFS was 17.1 months (95% CI: 10.8 - 23.0, Figure 1) and median OS was 48.0 months (95% CI: 22.6 months, not estimated, Figure 2). There was no significant effect of dose level on PFS or OS. Multivariable Bayesian survival time models found high-risk cytogenetics to be significantly harmful to both OS and PFS. In addition, degree of plasma cell infiltration of bone marrow before auto-HCT was significantly harmful to PFS.
Conclusion: Lenalidomide up to 100 mg PO daily x 7 can be safely combined with high dose melphalan and auto-HCT. Longer follow-up demonstrates PFS and OS as comparable to other salvage treatments for MM, suggesting that this regime can be applied as a part of the sequence of therapies for these patients.
OS of 48.0 months (95% CI: 22.6 months, not estimated; N=57, Deaths=28)
Orlowski:Takeda Pharmaceuticals: Research Funding. Champlin:Intrexon: Equity Ownership, Patents & Royalties; Ziopharm Oncology: Equity Ownership, Patents & Royalties.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal