Abstract
Introduction
Children and adolescents with Hodgkin lymphoma (HL) have excellent long-term outcomes after combined modality treatment, however ~15-20% will either relapse or have primary refractory disease. (Shankar A, BJH 2014) Salvage chemotherapy followed by autologous stem cell transplantation (ASCT) is the standard of care for many pediatric patients with relapsed HL.
In adults, achieving a complete remission by functional imaging (FI), particularly positron emission tomography (PET), after salvage chemotherapy is a strong predictor of outcome after ASCT. The majority of published data in pediatric cohorts has employed computed tomography (CT) measurements to assess pre-transplant disease status. We report pre-ASCT FI and clinical outcomes of 49 consecutive children/adolescents, who underwent ASCT for relapsed/refractory HL at our institution.
Patients and Methods
Following IRB approval, the records of 49 patients with relapsed/refractory HL who received ASCT from January 1, 2001 to December 31, 2014 were reviewed. All had PET (43) or gallium (6) at time of relapse and subsequent time points in disease evaluation pre-ASCT. Available PET scans were reviewed by 2 nuclear medicine physicians, blinded to the clinical data, and assigned Deauville scores. 12 patients who did not have available PET images had outside reports documenting negative PET upon completion of initial salvage therapy. Negative FI was defined as interval resolution of previous gallium avid disease, documented negative PET, or Deauville score ≤ 3.
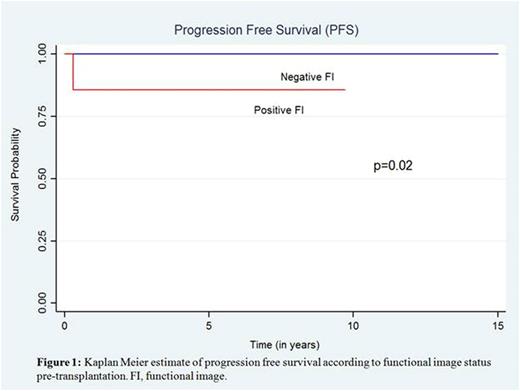
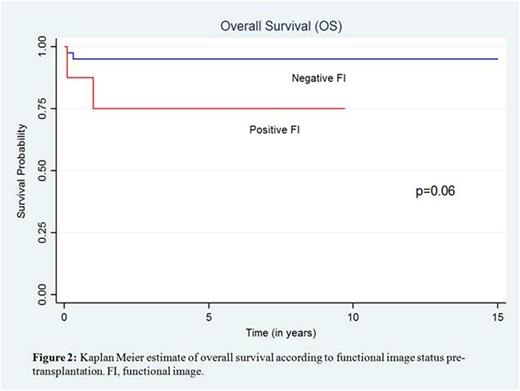
Relapse therapy regimens varied. Patients received standard conditioning regimen with carmustine, etoposide, cytarabine and melphalan(BEAM) followed by stem cell infusion. Post-transplant radiation therapy (RT) was given if no prior RT to the site(s) of relapse. Overall survival (OS) was measured from the date of transplant to death from any cause, progression free survival (PFS) defined as a relapse of HL, with non-HL-related deaths censored. (Lieskovsky JCO, 2004) OS and PFS distributions were examined using Kaplan-Meier curves and the differences between groups were analyzed using the log-rank test and a significant P value < 0·05.
Results
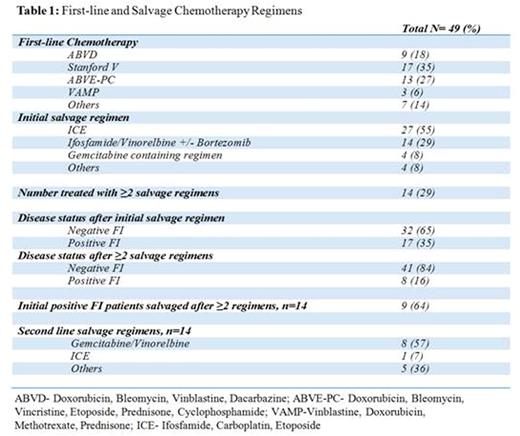
Median age at time of transplant was 16.4 years; 55% of patients were males. Eighteen (37%) had refractory disease, 22 (45%) relapsed early (3-12 months from completion of primary therapy) and 9 (18%) relapsed late (>12 months).Thirty-one (63%) relapsed within initial RT field. First-line and salvage therapy regimens are detailed in Table 1. Fourteen (27%) received ≥2 salvage therapies; 3 had a 3rd line agent. Nine of the 14 (64%) later achieved negative FI. Three patients with positive PET after initial salvage therapy did not receive a 2nd line regimen. Pre-ASCT,41 patients (84%) had negative FI vs 8 (16%) with positive FI. Eighteen patients (37%) received post-transplant RT; including 5 (64%) in the positive FI group and 13 (32%) in the negative FI group. Median duration of follow up post-transplant was 45.6 months (1-180 months).
Forty-five patients were alive and disease-free at last follow up. Post-transplant events included 2 early deaths from transplant-related complications, 1 motor vehicle accident and 1 relapse 6 months post-transplant (pre-transplant Deauville score of 5, death at 12 months). No patient developed a second malignancy. 3-year OS for entire cohort was 92% (95% CI 78-97) with PFS of 98% (95% CI 86-99). 3-year PFS was 100% vs 86% (95% CI 33-98) in negative and positive FI groups respectively (p=0.02). 3-year OS for negative and positive FI patients was 95% (95% CI 82-99) vs 75% (95% CI 31-93) respectively (p=0.06). Complete remission by FI after initial salvage therapy was associated with a trend in OS (97% vs 82% in those with persistent disease) (p=0.08) but not PFS. Extra-nodal disease at relapse, refractory disease and radiation-field relapse had no significant impact on either OS or PFS in a univariate analysis. Cox proportional hazard ratios could not be performed on multivariate analysis given rarity of events.
Conclusion
Our analysis revealed outstanding outcomes for children/adolescents with relapsed/refractory HL. Negative pre-ASCT PET or gallium was associated with excellent PFS and OS but there were too few relapses to identify the predictive value of pre-transplant FI. Patients who do not achieve complete metabolic response to second line salvage therapy may be candidates for novel approaches.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal