Abstract
Introduction
Autologous hematopoietic transplantation (AHT) is an established therapy in multiple myeloma (MM) and lymphoma. Standard mode (CRYO) consists on collection of autologous precursors, freezing with dimethyl sulfoxide (DMSO) and subsequent thawing and reinfusion. However, this process is toxic and increases transplantation costs. Non-Cryopreserved (Non-CRYO) mode is a less expensive mode of AHT that has shown same transplantation outcomes in several single-center experiences. The Pontificia Universidad Católica de Chile transplant program began Non-CRYO AHT in 2015. In this study, we have compared patients who had Non-CRYO AHT in Chile with patients who had standard CRYO AHT in Spain at the same period of time.
Aims: Our main objective was to compare short-term complications between both modes of AHT in terms of severe mucositis measured by use of morphine, total parenteral nutrition requirements, febrile neutropenia, engraftment and length of hospitalization. Other objectives were overall response, non-relapse mortality and overall survival.
Methods.
This is a prospective analysis of all consecutive adult patients treated with AHT in both centers from January 2015 to May 2016. CRYO mode procedure consisted of the stimulation of hematopoietic progenitors with filgrastim +/- plerixafor in both MM and lymphoma patients, CD34-apheresis on day 5, freezing of product with DMSO, subsequent thawing and reinfusion post conditioning. In Non-CRYO mode, once patients achieved the best response, they received the same filgrastim +/- plerixafor treatment followed by CD34-apheresis without DMSO freezing. Apheresis product was kept at 5°C during conditioning and then re-infused. Conditioning regimen for MM patients was high dose melphalan and for lymphoma patients BEC or BEAM protocols. All patients were hospitalized during the period of pancytopenia and received transfusions, antibiotics and symptomatic measures as usual. Patients were discharged when they reached >500 neutrophils/uL and 25.000 platelets/uL without the need of transfusions, and did not have active infections.
Results.
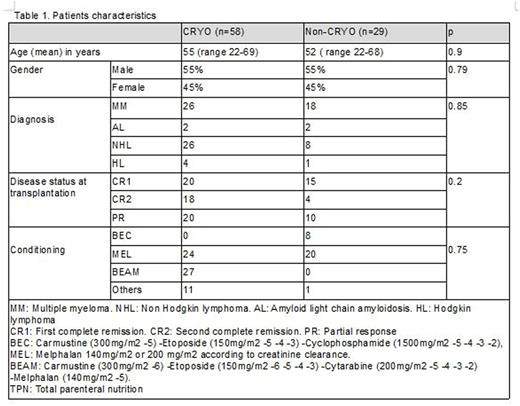
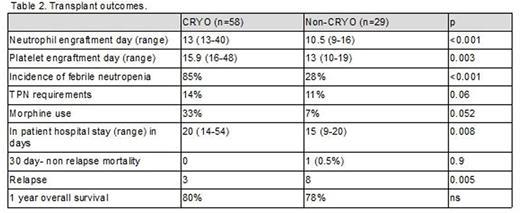
Since 2015, 29 Non-CRYO and 58 CRYO AHT were performed in both centers. General characteristics are detailed in table 1. No significant differences were observed regarding demographic characteristics, basal disease and status, and CD34 cellularity. 7AAD FACS viability at infusion day was greater than 92% in Non-CRYO and all patients engrafted in both groups. As we show in table 2, neutrophil and platelet engraftments were significantly earlier in Non-CRYO group vs CRYO group (p = 0.003). Less gastrointestinal toxicity was seen in Non-CRYO group in terms of morphine use (11% vs 55%, p= 0.001) and total parenteral nutrition requirements (11% vs 14%, p= 0.06). The incidence of febrile neutropenia was lower in Non-CRYO group (28% vs 85% respectively, p=0.0001). Finally, lengh of hospitalization was shorter in Non-CRYO (p=0.008). Overall response obtained after transplant was similar in both groups. Non relapse mortality was low and similar in both groups (0 vs 0.5%). We found no differences in relapse nor overall survival.
Conclusions.
This analysis demonstrates a clear advantage of Non-CRYO AHT over CRYO AHT in terms of short term complications, in particular, faster engraftment, shorter hospital stay and lower incidence of febrile neutropenia and severe pain manifested by morphine use. These data are especially relevant to transplant centers with high flow of patients or limited resources. The savings in costs of freezing process and shorter hospitalizations should be evaluated in further investigations.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal