Abstract
Introduction: With improvements in supportive care, including graft-versus-host disease (GVHD) control, relapse has become the major complication of allogeneic BMT. The use of haploidentical donors often allows the potential to select a different donor for the second transplant. We examined the outcomes of patients who underwent a second BMT for relapse at Johns Hopkins between 2005 and 2014. We hypothesized that if loss of heterozygosity is a mechanism for relapse after haploBMT, then utilizing a donor that recognizes the other shared haplotype could improve antitumor activity and thus overall survival (OS). In the case of a failed matched transplant, recognition of a non-shared haplotype on the tumor by the second allograft would be beneficial.
Methods: We identified all patients who received a second transplant for relapse of a hematologic malignancy between 2005 and 2014. Acute GVHD (aGVHD) is reported as Glucksberg grades 1-4; chronic GVHD (cGVHD) is reported as limited or extensive. GVHD and non-relapse mortality (NRM) was calculated via cumulative incidence (CI) with competing risk analysis. OS was calculated as the time from second transplant to death or last known follow-up and estimated using the Kaplan Meier method. Differences in time to death between patient groups were estimated using Cox proportional hazards models. Non-relapse mortality was estimated using Fine and GrayÕs method.
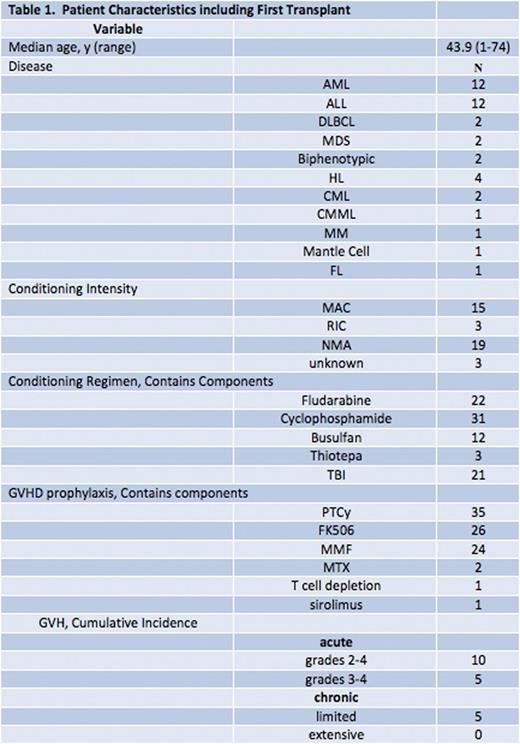
Results: Between 2005 and 2014, 40 patients received a second BMT for a relapsed hematologic malignancy (Table 1). The median age at second transplant was 43.9 (range 1 to 74); 14 (35%) were female. Fifteen (41%) received myeloablative conditioning for their first transplant, and 35 (92%) received high dose post-transplant cyclophosphamide (PTCy) as part of their GVHD prophylaxis. The incidence of grade 2-4 aGVHD after the first transplant was 13%, and limited cGVHD was 13%. There was no extensive cGVHD.
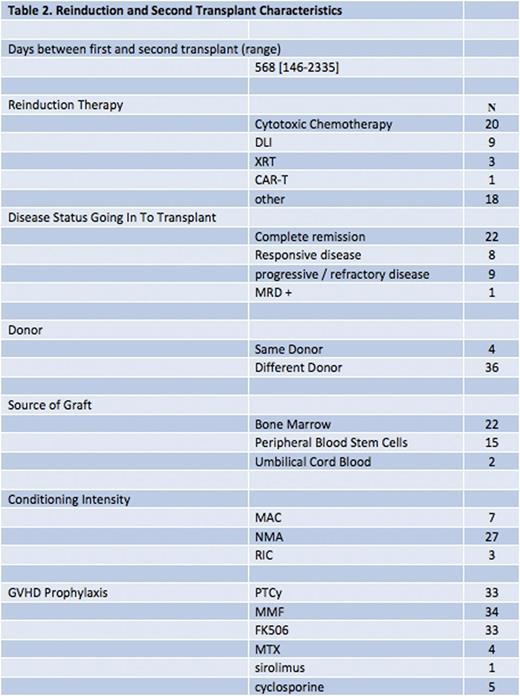
Re-induction therapy and second allograft characteristics (Table 2): Refractory or progressive disease at the time of second transplant was present in 20% of patients, and 7/40 (18%) had their second transplant within 1 year. After a first failed HLA-matched transplant, 15 received a haploidentical graft, and 4 received a second HLA-matched graft. Among the 21 who relapsed after a haploBMT, 7 received an HLA-matched allograft, and 14 received a haploidentical graft; 6 out of those 14 used a donor that switched the shared haplotype. Most (81%) received PTCy with the second BMT.
Median follow up is 598 days. Median OS in the cohort is 911 days (95% CI 602 Ð NR); 4 year OS is 38%. The CI of NRM by 2 years was 29% - 4 patients died of complications of GVHD (only one of whom received post-transplant Cyclophosphamide), 3 associated with prolonged cytopenias, 1 within a month of BMT, and 3 of pneumonia. Grade 2-4 aGVHD occurred in 11 pts (28%), grade 3-4 in 5 (13%). Extensive cGVHD was seen in 7 (18%).
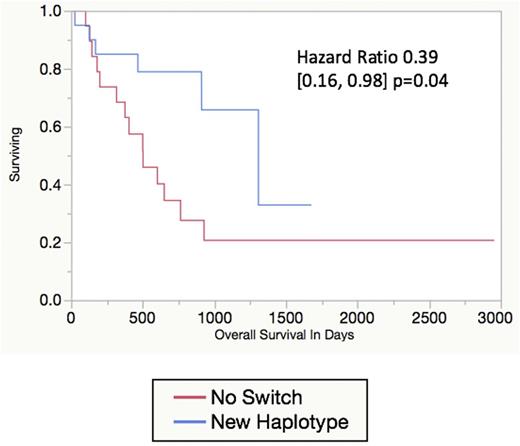
Median OS for the patients who relapsed after initial haploBMT who were then retransplanted with an HLA-haploidentical donor with a different shared haplotype has not been reached, versus a median OS of 501 [317-2950+] days among the 15 who did not receive a graft with an alternate shared haplotype (HR 0.21 [0.03, 1.61]; p=0.06). If the 19 patients who received a matched allograft at first transplant are included, median OS is 552 days in the group transplanted with a second graft with the same shared haplotype(s), and 1308 days (Figure 1) in the group whose allograft contained a different non-shared haplotype (HR 0.39 [0.16, 0.98]; p=0.04).
OS was better when the second transplant was performed more than one year after the first (HR 0.30 [0.11, 0.80]; p=0.03). A trend towards improved OS was associated with disease status at time of second transplant (remission or chemo-responsiveness versus progressive or refractory disease; HR 0.41 [0.16, 1.03]; p=0.07). Source of graft (BM versus peripheral), conditioning intensity, era of transplant (2005-2010 versus 2010-2015), same versus different donor, and age group (<25, 25-60, 60+) did not significantly influence OS.
Conclusion: Second transplants are feasible in all age groups and provide a reasonable chance of long-term survival. GVHD rates using PTCy are low, and similar to that seen with first BMTs. An allograft sharing a different haplotype in the case of relapse after haploBMT, or a haploidentical donor after failure of a matched graft, may be beneficial.
OS by Second Donor Haplotype
Brodsky:Apellis Pharmaceuticals Inc: Membership on an entity's Board of Directors or advisory committees; Alexion Pharmaceuticals Inc: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Achillion Pharmaceuticals: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal