Abstract
The process of allogeneic hematopoietic cell transplantation (HCT) is often associated with poor oral intake and as a result, nutritional status declines. Although it might seem obvious that optimal nutrition is likely to improve outcomes of transplantation, there are no clinical data that directly support this assumption. It is also unclear whether artificial nutrition support (ANS) should be provided as enteral tube feeding (ETF) or parenteral nutrition (PN).
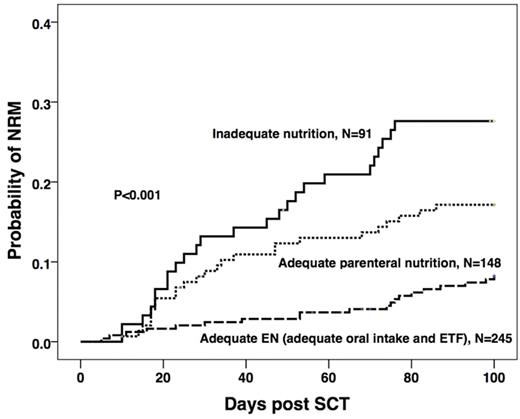
In this study we analysed day 100 non-relapse mortality (NRM) and incidence and severity of acute graft versus host disease (GvHD) according to both the route and adequacy of nutritional intake together with other known prognostic factors. A total of 484 patients who underwent HCT for hematological malignancy at a single institution between 2000 and 2014 were included. Myeloablative conditioning was used in 285 (59%) patients, 272 of whom received a TBI based regimen. Reduced intensity conditioning was given to 199 (41%) patients. For the 236 (49%) unrelated donor cell recipients in vivo T-cell depletion with alemtuzumab was used. Myeloablative HCT recipients were advised to have an enteral feeding tube inserted prophylactically at day 1 post HCT. ANS was initiated in 228 (47%) patients who met pre-defined feeding criteria that include actual or anticipated oral intake below 1/3 of estimated requirement for 5 or more days or significant weight loss or low body mass index. Total of 245 (51%) patients had adequate enteral nutrition (EN) either orally (N=198) or with use of ETF (N=47). Patients in whom ETF could not be established received PN (N=148, 31%) in order to provide adequate nutrition. The remaining 91 (19%) patients had inadequate nutrition due to either curtailed ANS (N=33) or a failure to start ANS because of a lack of feeding access via any route (N=58).
The effects of patient, disease and transplant factors were studied in univariate analyses on NRM, acute GvHD and engraftment, following which multivariate analyses showed significant associations of NRM with age > 50 years (hazard ratio (HR) 2.3; 95% confidence interval (CI) 1.4 - 3.7; P=0.001); previous autograft (HR 2.4; 95% CI 1.3 - 4.5; P=0.007) and positive recipient CMV serology (HR 1.9; 95% CI 1.1 - 3.2; P=0.019). In addition, HRs were significantly increased in the PN and inadequate nutrition groups compared to those with adequate enteral intake: adequate PN: HR 3.2; 95% CI 1.7 - 6.0, inadequate nutrition: HR 4.4; 95% CI 2.4 - 8.0; all P<0.001 (Figure). There were increased incidences of gastrointestinal GvHD of any stage and acute GvHD > grade 1 in patients who received PN (HR 2.0; 95% CI 1.2 - 3.3; P=0.006, and HR 1.8; 95% CI 1.1 - 3.0; P=0.018, respectively), but not in those with inadequate nutrition compared to adequate EN. Other significant covariates in the model for both increased overall and gut GvHD were the use of myeloablative versus reduced intensity conditioning P=0.001 and P<0.001 and female donor to male recipient versus other combinations P=0.047 and P=0.025 respectively.
In conclusion the data show that adequate nutrition during allogeneic HCT is associated with improved non-relapsed mortality at 100 days. Adequate EN is associated with significantly better results for this outcome than adequate PN. Furthermore adequate EN, predominantly via oral intake may be associated with lower incidence of overall and gut GvHD when compared to PN, perhaps because of its ability to maintain gut mucosal integrity and for support of the gastrointestinal tract environment, including gut microflora. Although the retrospective nature of this study can only indicate association, the significant hazard ratios reported warrant further research into optimising enteral nutrition in recipients of HCT.
Milojkovic:Novartis: Honoraria; Bristol Myers Squibb: Honoraria; Pfizer: Honoraria; Ariad: Honoraria. Apperley:Incyte: Speakers Bureau; Novartis: Honoraria, Speakers Bureau; Pfizer: Honoraria, Speakers Bureau; Bristol Myers Squibb: Honoraria, Speakers Bureau; Ariad: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal