Abstract
Introduction: Ex-vivo CD34+ selected allogeneic hematopoietic cell transplantation (alloHCT) after myeloablative conditioning (MAC) has been successfully utilized in the treatment of hematologic malignancies, with high rates of survival and a reduced incidence of graft-vs-host disease (GVHD). However, as MAC is associated with higher toxicity than reduced intensity conditioning (RIC), a comprehensive evaluation of toxicities and the effect on survival and non-relapse mortality (NRM) within the first year (yr) after myeloablative allo-HCT is necessary.
Methods: Toxicities (≥ grade 3 by CTCAE 4.0) were retrospectively collected on 200 pts within the 1st yr of alloHCT (CD34+ selection with the ClinicMACS® CD34 Reagent System) after MAC from 2006-2012. Individual toxicities were organized into 91 toxicity categories and further into 17 organ-based groups. One toxicity per group per specified time period was used for statistical analyses. Overall survival (OS) and NRM were calculated using Kaplan Meier methods, and Cox regression was used for univariate analysis of risk of toxicities and survival outcomes across patient and treatment characteristics.
Results: 200 pts (median age 57, range 19 -73) were included in the study. Indications for HCT were AML/ALL/MDS (n=144, 72%), multiple myeloma (n=30, 15%), other (n=26, 13%). Donors were MRD or MMRD (n=77, 38%), MUD (n=78, 39%) or MMUD (n=45, 23%). Median HCT-comorbidity index (HCT-CI) score was 2 (0-10). MAC was chemotherapy (n=144, 72%) or total body irradiation (TBI, n=56, 28%) based. The follow up period for surviving pts was 12 months. At day 100, 23 pts (11.5%) experienced grade 2-4 acute GVHD, while 6 pts (3%) developed grade 3-4 acute GVHD.
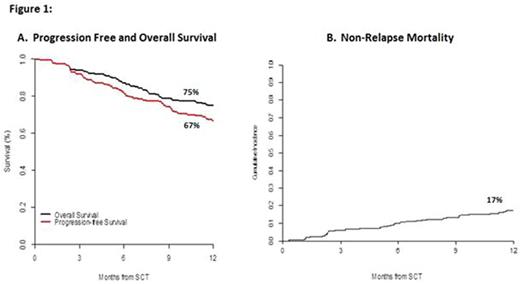
The 5 most common grade > 3 toxicities, with associated cumulative incidences by day 365, were infection (0.91, 95% CI 0.86-0.94), metabolic (0.91, 0.86-0.94), hematologic (0.87, 0.81-0.91), oral/ gastrointestinal (GI) (0.66, 0.59-0.72), and pulmonary (0.24, 0.18-0.30). At 1 year post alloHCT, OS and progression-free survival (PFS) for the cohort were 75% and 67%, respectively (Fig 1A). The median number of toxicities at day 100 was 6. Pts experiencing >6 toxicities at day 100 had the same 1yr OS as pts with < 6 toxicities (80%, p=0.92). NRM was 17% at 1 yr (Fig 1B).
Univariate analysis of risk factors identified associations with common toxicities occurring in the 1st yr. While no specific factors increased the risk of infection, age and male gender were associated with a decreased risk [HR 0.98 (0.97-1.0), p=0.02, HR 0.6 (0.47-0.78), p=0.002 respectively]. Patients with a high absolute lymphocyte count (ALC) [HR 0.41 (0.26 to 0.63), p= <0.001] had a decreased risk of hematologic toxicity. The use of TBI in the conditioning regimen conferred a higher risk of GI toxicity [HR 1.76 (1.22 to 2.53), p= 0.002], while age [HR 0.97 (0.96 to 0.99), p= .001], male gender [HR 0.58 (0.41 to 0.82), p=0.002], URD [HR 0.67 (0.47 to 0.95), p=0.023] and high ALC [0.57 (0.35 to 0.93), p=0.024] were associated with a decreased risk. Hepatic complication risk rose in pts with a ferritin level >2500 [HR 3.46 (1.9 to 6.32), p= <0.001].
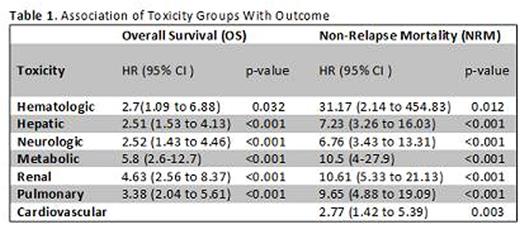
Decreased OS was seen in CMV+ pts [HR 1.82 (1 to 3.29), p=0.049]. Busulfan levels > target [HR 2.79 (1.32 to 5.91), p= <0.001] and HCT-CI >3 [2.45 (1.08 to 5.57), p=0.01] increased the risk of death and NRM [HR 3.09 (1.33 to 7.18), p=0.001, HR 3 (1.03 to 8.7), p=0.02] respectively. Factors such as age, male gender, male donor, disease type, URD, CMV+ donor, TBI, palifermin use, and albumin levels did not impact OS or NRM. Table 1 summarizes individual toxicity groups associated with OS and NRM.
Conclusion: In the 1st yr after MAC alloHCT, pts experienced grade > 3 hematologic, metabolic, infectious, GI and hepatic complications, which would be expected with MAC. This is consistent with BMT-CTN data indicating CD34+ grafts with MAC seem to be associated with similar >3 toxicities as unmanipulated grafts. Further toxicity may be related to methotrexate and calcineurin inhibitors used in conventional transplants. The pts in this analysis still exhibited high OS and PFS with a low rate of acute GVHD. This analysis can contribute to identifying toxicities and methods to mitigate them through patient selection and post alloHCT management. These results are also highly relevant to the ongoing prospective exploration of CD34+ selection in pts with hematologic malignancies in the BMT-CTN 1301 randomized phase 3 trial.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal