Abstract
Introduction: The tumor micro-environment poses a limitation to the efficacy of adoptive NK cell therapy due to several immunosuppressive cytokines. TGF-beta, produced in excess by tumor cells, regulatory T cells and stromal cells, facilitates epithelial to mesenchymal transformation thereby promoting metastasis and fibrosis. This high TGF-beta milieu in cancer patients also impairs innate natural killer (NK) cell mediated cancer immunity through various mechanisms.
Adoptive transfer of healthy donor NK cells will have limited clinical efficacy when highly activated NK cells are introduced into the immunosuppressive TGF-beta rich tumor microenvironment of cancer patients. We are testing several small molecule inhibitors of the TGF-beta receptor in combination with healthy donor NK cells with a goal of enhancing adoptive NK cell therapy in various disease models.
Methods: Human NK cells isolated from healthy donor peripheral blood were expanded over a 21-day period in co-culture with irradiated K562 cells genetically modified to express membrane-bound IL-21. (Somanchi et al. 2011 JoVE 48. doi: 10.3791/2540). Cell culture media was supplemented with IL-2 (50mU/mL).
For in vitro assays, at the beginning of expansion week 3 the culture conditions for NK cells was continued unchanged, supplemented with TGF-beta 1 ligand (TGF-B1) at 5ng/mL or 10ng/mL either alone or in combination with EW7197 (a TGF-beta Type 1 receptor inhibitor) or with EW7197 alone. These NK cells were tested with Calcein-AM release cytotoxicity assays at various time points from addition of TGF-B1 (0h, 36h, 72h and 96h). Briefly, NK cells were co-cultured with OCI-AML cells labeled with Calcein-AM at a ratio of 5NK:1 OCI-AML. At the end of 4 hours co-incubation, cytotoxicity was measured by relative fluorescence of calcein release into the culture supernatant compared with Triton-X induced complete target cell lysis.
In a murine liver metastases model using the colon cancer cell line HCT116, 105 HCT116 cells were surgically implanted into NSG mouse spleens (following hemi-splenectomy). Mice in 2 groups (3/group) subsequently received 5 x 106 NK cells each (tail vein), weekly for two weeks, starting 10 days post-op. Another control group received vehicle infusions alone while a fourth control group received the TGF-beta inhibitor LY2157299 by oral gavage twice daily at 75mg/kg for two weeks. One group of mice receiving NK cells also received twice daily LY2157299 for two weeks starting with the first NK cell infusion. Mice receiving NK cells also received IL2 (75,000U IP) three times a week for two weeks.
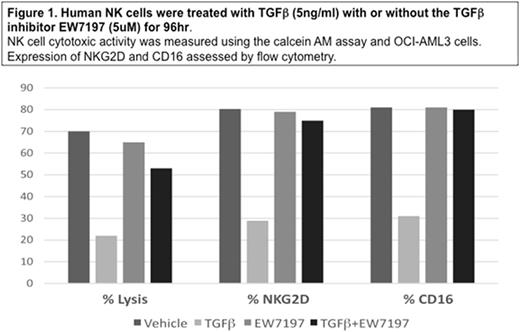
Results: At TGF-beta levels similar to that found in AML patients (5ng/ml), NK cell killing of OCI cells was markedly impaired progressively from 36h to 96h exposure. This reduced cytotoxic activity correlated with a 3-4 fold decrease in expression of NKG2D most marked at 96h(Figure 1). CD16 expression was also significantly reduced by 2-3 fold on TGF-beta exposed NK cells after 96h. The TGF-beta inhibitor EW7197 maintained NK cell killing as well as NKG2D and CD16 expression in the presence of TGF-B1 (Figure 1).
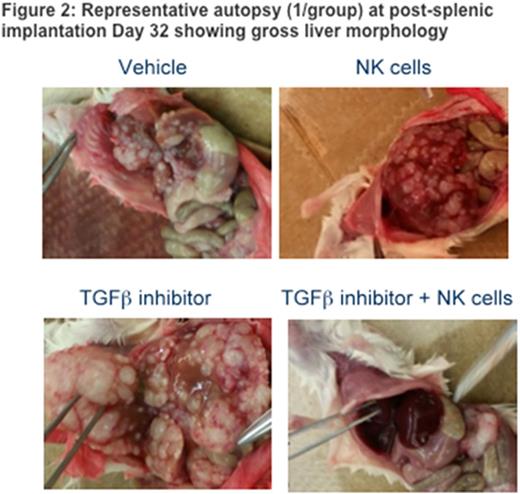
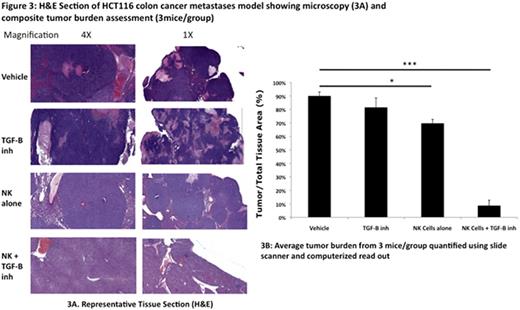
At 32 days post-splenic implantation, vehicle mice (those that received HCT116 either alone or in combination with LY2157299 alone) appeared moribund and had grossly distended abdomens with ascites. All mice were autopsied at this time point. All control mice had grossly enlarged livers with significant metastases and absence of viable liver tissue (Fig 2). In contrast, mice treated with two weekly infusions of NK cells and LY2157299 for 4 weeks had no ascites and predominantly healthy livers. All mice that received NK cells alone had some evidence of liver metastases with various degrees of disease burden. Composite H&E stains of liver sections from 3 mice/group showed <10% liver metastases microscopically in mice treated with a combination of NK cells and LY2157299. This was significantly reduced compared to 80-90% in the untreated or LY2157299 alone mice and 60-70% in the NK cell alone group (Fig 3).
Discussion: Our preliminary results indicate that TGF-beta inhibition in combination with adoptive NK cell therapy can mitigate the immunosuppressive tumor microenvironment conferred by TGF-beta signaling. We are in the process of validating this approach in other preclinical models of both hematologic malignancies and solid tumors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal