Abstract

Introduction: In the CRASH II trial, administration of tranexamic acid (TXA) >3 hours after injury was associated with increased mortality. Recent evidence indicates that fibrinolysis inhibition upon presentation to the emergency department (ED) is associated with increased mortality from organ failure. However, it remains unclear if fibrinolysis status changes in response to resuscitation. We hypothesize that the incidence of fibrinolysis resistance (shutdown) increases after resuscitation and is associated with increased post injury complications, prolonged respiratory failure, and prolonged ICU stay.
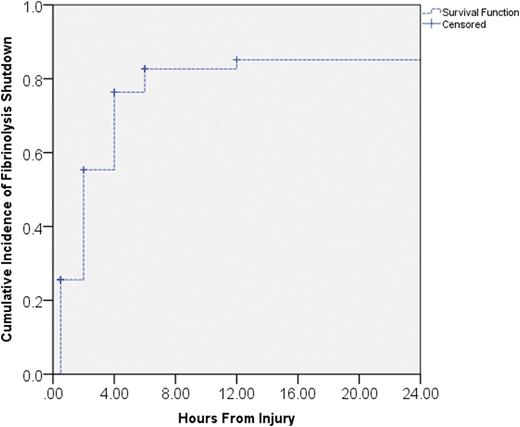
Methods: Blood samples were collected prospectively on injured patients with documented prehospital shock (SBP < 90mm HG ) identified by the emergency medical service as part of an ongoing study to measure the impact of resusciation on coagulation in trauma. Patients had thrombelastography (TEG) samples drawn at admission and sequentially over 24 hours. Susceptibility to fibrinolysis was quantified using a tissue plasminogen activator (tPA) modified TEG. Fibrinolysis shutdown was defined as the lysis at 30 minutes (LY30) < 5thpercentile of healthy volunteers (n=160). Kaplan-Meier plot was generated to identify the timing and cumulative incidence of fibrinolysis shutdown in the first 24 hours after injury. Outcomes were contrasted between patients with and without shutdown at different time intervals from injury using a Mann Whitney U test to assess for 30 day post-injury complications, mechanical ventilator free days, and intensive care unit free days. A nested population of twelve patients that had elevated fibrinolysis activity on presentation to the emergency department and did not receive TXA were analyzed for endogenous tPA and plasminogen activator inhibitor-1(PAI-1) activity during their first 24 hours post injury, which also including pre hospital samples before resuscitation.
Results: Ninety patients (median ISS of 27 and prehospital SBP of 72 mmHG) were included in the analysis, with a mortality rate of 13%. Overall, 76 % of patients developed fibrinolysis shutdown. Fifty percent of the population developed fibrinolysis shutdown within 2 hours of injury, and 75% of patients reached shutdown by 4 hours post injury (figure 1). Patients who remained in shutdown at 12 hours postinjury had significantly fewer ventilator free days (median 23 vs 26 p=0.005) and fewer ICU free days (median 20 vs 26 p= 0.004) with longer hospitalization (median 16 days vs 5 p=0.001). Patients in shutdown at 12 hours also had an increased incidence of in hospital complications (40% vs 15% p=0.048). Patients that were in fibrinolysis shutdown at 12 hours had increased plasma (p=0.010) platelet (p=0.007) and TXA (p=0.033) transfusions in the first 6 hours of resuscitation compared to those patients not in shutdown. In the nested cohort of patients with elevated LY30 upon presentation to the hospital, the median tPA activity peaked in prehospital samples (median 0.87 IU/ml) and decreased 10 fold by 4 hours postinjury (0.08 p<0.001), whereas PAI-1 activity increased 700 fold during the same time frame (0.04 to 175 IU/ml p<0.001).
Conclusion: Fibrinolysis resistance becomes prevalent in injured patients with prehospital hypotension after successful resuscitation, and this is associated with markedly elevated levels of PAI-1. Patients with fibrinolysis shutdown 12 hours after injury have increased ventilator requirements and prolonged ICU stays. Extending the time patients are in fibrinolysis shutdown during the post resuscitation period appears to be a risk factor for protracted respiratory failure, and may explain why delayed administration of TXA is associated with increased mortality. These results suggest future therapeutic opportunities to reduce PAI-1 activity in the postinjury period to attenuate postinjury organ failure.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal