Abstract
Objective: Baseline quantitative PET parameters measuring tumour burden and metabolism are proposed as early prognosticators of outcome in different lymphoma subtypes. It has been shown that in advanced stage Hodgkin lymphoma (HL) and Primary mediastinal B cell lymphoma, total metabolic tumor volume (TMTV) or total lesion glycolysis (TLG) predicted outcome better than the bulk. From the H10 EORTC/LYSA/FIL randomized intergroup trial (NCT00433433) including patients with supradiaphragmatic stage I/II, histologically proven classical HL, we investigated the prognostic value of quantitative PET metrics measured on baseline FDG PET/CT in the unfavorable group of the standard arm.
Methods: One hundred and fifty patients were randomly selected from the 352 patients recruited by the LYSA centers, in the unfavorable group (≥ 4 nodal areas or age ≥ 50 yrs or mediastinal thoracic (MT) ratio ≥ 0.35 or erythrocyte sedimentation rate (ESR) ≥ 50 (without B-symptoms) or ESR ≥ 30 (with B-symptoms)) of the standard arm of the H10 trial. Only patients who had baseline PET/CT with fused images available were analyzed. Standard treatment was 4 cycles of ABVD completed by involved-node radiotherapy. All patients had an interim PET performed after 2 ABVD cycles (PET2). Baseline TMTV was computed using the 41% and 25% SUVmax thresholding methods; SUVmax, TLG41%, TLG25% were calculated. PET2 was centrally reviewed reported. Optimal quantitative parameters cut-off to predict PFS and OS were determined by ROC curves, and Kaplan Meier (KM) curves were obtained. Multivariate analyses were performed using a Cox model.
Results: 128 patients with a median age of 32 years were analyzed: 54 (42%) had B symptoms, 74 (58%) had ESR>40 (ROC optimal cut off), 48 (37%) mediastinal bulk as defined above. Median TMTV41%, TMTV25%, SUVmaxand TLG41%, TLG25%were 81 cm3 (25th-75thpercentiles 44-145 cm3), 194 cm3 (112-323), 11 (8-14), 407 cm3 (221-475) and 731 cm3 430-1321) respectively. After a median follow-up of 5 years, the 5y-PFS was 84% and the 5y-OS was 92%.
The strongest PET quantitative parameter to predict outcome was the TLG41% (p=0.0006 HR=6.5 for PFS with a cut off of 420 cm3, p=0.025 HR=7.7 for OS with a cut off of 584 cm3). Patients with a high TLG41% had a 5y-PFS of 76% vs 92% (95%CI 71-81; 88-96) and a 5y-OS of 88% vs 96% (95%CI 83-92; 92-100) for those with the lower TLG41% respectively. Similar results were found using 25% SUVmax threshold (p=0.0005 HR=4.7 for PFS, p=0.0032 HR=7.9 for OS).
TMTV41% higher than 149 cm3 cut off was associated with a worse PFS (p=0.0099, HR=3.26) and OS (p=0.022, HR=4.8) but with a lower significance level. A SUVmax greater than 14 was also associated with a worse PFS (p=0.018 HR=3.0) with a 5y-PFS of 74% vs 86% but not with OS. In multivariate analysis testing TLG41% and SUVmax or TLG41%and TMTV41%, only TLG41% remained significant (p=0.0096 and p=0.015 for PFS and OS respectively).
B symptoms and ESR>40 were predictive of PFS (p=0.0077 HR=3.7 and p=0.0062 HR=6.07 respectively) but not of OS. MT ratio was predictive of neither PFS nor OS (p=0.49, p=0.20). In multivariate analysis, B symptoms, ESR>40 and TLG41% remained significant independent predictors of PFS (p=0.038; p=0.034; p=0.014 respectively).
For the 124 patients with a centralized reading available, a positive PET after two cycles (PET2 +) using IHP criteria (n=29) was associated with a worse PFS (p=0.0006). In multivariate analysis testing TLG41% and interim PET, they both remained independent prognosticators (p=0.014 and p=0.025 respectively).
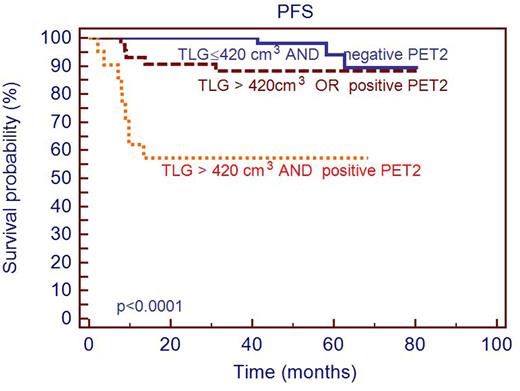
Interestingly combining TLG41% and interim PET brings out 3 distinctive prognostic categories (p<0.0001): negative PET2 and low TLG41% with good outcome (5y-PFS=92%, n=60); positive PET2 and high TLG41% with bad outcome (5y-PFS=57%, n=21) and an intermediate category (5y-PFS=88%, n=43) cf. KM curve. No progression was observed in the 8 patients with a positive interim PET but a low baseline TLG41%, suggesting that TLG41% results may reduce the numbers of false positive PET2 patients.
Conclusion: Quantitative PET parameters improve patient risk stratification at staging. The study data suggest that TLG is an independent prognosticator of outcome and seems particularly interesting in early stage HL patients, to identify in conjunction with the early PET response, those patients who require treatment intensification.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal