Abstract
Background
It is of great importance to know the impact in quality of life (QOL) after allogeneic hematopoietic stem cell transplantation (allo-HSCT) according to types and severity of chronic graft-versus-host disease (GVHD), to care for physical, mental and social aspects of transplant survivors. We conducted a cross-sectional questionnaire study to examine the relationship between patient-reported QOL and chronic GVHD defined by National Institute of Health (NIH) criteria. We also investigated the degree of agreement between visual analogue scales provided by patients (VASpt) and physicians (VASdoc).
Methods
The protocol was approved by the Institutional Review Board at each of the participating centers, and all subjects provided informed consent in accordance with the Declaration of Helsinki. Patients enrolled in the cohort were identified in the national transplant registry database registered from 47 centers which participated this study. Eligibility criteria included recipients of allo-HSCT for hematological diseases between 1995 to 2009, who were aged 16 years or above at transplant and 20 years or above at survey, and were relapse-free at survey. A total of 3301 eligible patients were registered in the database.
SF-36, FACT-BMT, and VAS were administered to assess patient-reported QOL. Physicians evaluated the types and overall and organ-specific severity grades of chronic GVHD defined by NIH criteria (skin, mouth, eyes, gastrointestinal tract, liver, lung symptom, pulmonary function tests [PFT], joint and fascia, and genital tract), oral administration of immunosuppressant (IS), and VAS of respective patients at survey.
Multivariable models were constructed to examine the relationship between QOL scores and types and severity of chronic GVHD after controlling for background covariates. Adjusted mean scores for the SF-36 summary scores were obtained as norm-based scores (mean=50, SD=10 based on general population). Interclass correlation coefficient (ICC) was obtained to evaluate the degree of agreement between VASpt and VASdoc. Data were analyzed with SPSS statistical software.
Results
In 1250 patients who were informed of the study, consent was obtained from 1216, and 1149 patients returned the questionnaires. Nine patients were excluded because of a time lag (>4 months) that patient/physician completed reports, consequently, 1140 pairs of patient's and physician's questionnaires were included in the analysis. Males accounted for 52%, the median age at survey was 51 (range, 20-77), and the median time after allo-HSCT was 7.1 years (3.3-18.9). By the global severity score, 34% of patients had no GVHD, 29% mild, 25% moderate, and 9% had severe chronic GVHD. Frequently affected organs were eye (31%), skin (25%) and oral cavity (21%).
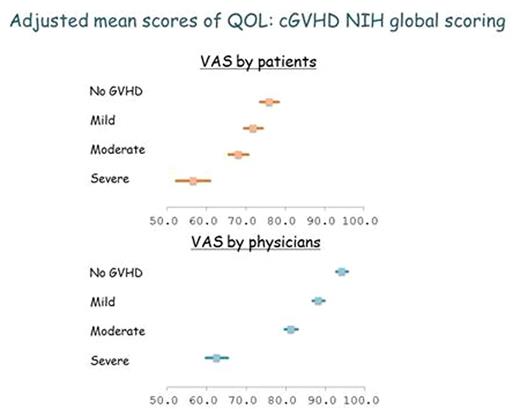
The median scores were 49.3 for physical component summary (PCS), 52.4 for mental component summary (MCS), and 52.3 for role/social component summary (RCS). Overall, VASdoc were higher than VASpt (median, 91.0 vs 75.6).
By the NIH global severity, PCS, FACT-BMT total score, VASpt and VASdoc were significantly (p<0.01) lower in mild compared to no GVHD, in moderate compared to mild, and in severe compared to moderate (Figure). MCS did not show significant differences between the NIH global severity grades. RCS was significantly lower in patients with severe chronic GVHD. In 8 of 9 organs (other than genital tract), mild chronic GVHD was associated with significantly lower PCS compared to no GVHD, and FACT total and VASpt were significantly lower in patients with mild GVHD in 7 of 9 organs (other than genital and PFT). Skin, oral and gut mild GVHD was associated with significantly lower MCS compared to no GVHD. The ICC for VASpt and VASdoc were remarkably low in patients with no or mild GVHD (0.0), while they were in fair agreement in patients with moderate (0.30) and severe GVHD (0.38). Patients who had IS at survey had a significantly lower QOL in all subscales. Compared to IS other than steroid, patients who had steroid at survey had significantly lower scores in PCS, RCS, and FACT-BMT total.
Conclusions
In long-term survivors after allo-HSCT, physical, role/social, and general QOL was impaired in patients with higher grades of chronic GVHD global scoring. Even mild chronic GVHD impaired patients' physical and general QOL in most types of GVHD. Physicians tended to underestimate changes in patients' QOL, especially for those with no or mild GVHD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal