Abstract
Primary myelofibrosis (PMF) is an age-related myeloproliferative neoplasm (MPN) characterized by progressive bone marrow fibrosis, increasingly ineffective hematopoiesis, vascular and inflammatory complications, and progression to acute myeloid leukemia (AML) in 20% of cases. PMF is the rarest and the most severe of MPNs, with unfavorable prognosis and challenging treatment. Constitutive activation of the JAK-STAT pathway is an essential contributor to the pathogenesis of PMF. Nonetheless, clinically available JAK inhibitors do not show consistent disease-modifying effects at the molecular and malignant stem cell levels, underscoring the need to identify other targetable pathogenic mechanisms in PMF and related MPNs.
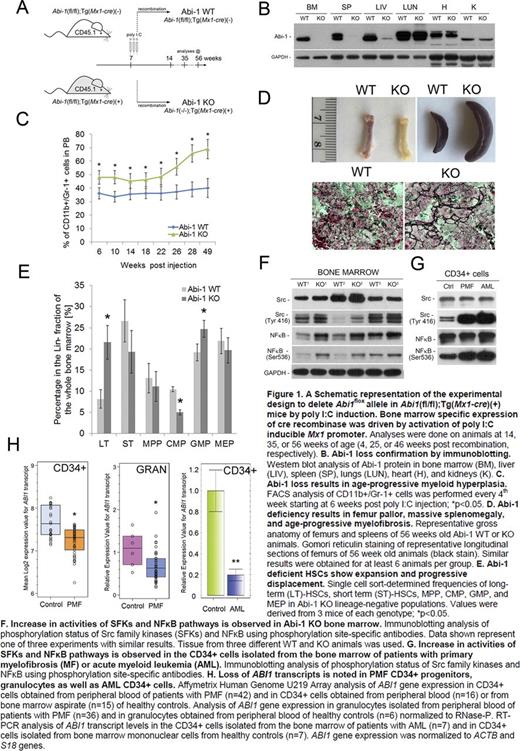
We recently described a new signaling cascade involved in the maintenance of the malignant phenotype of stem cells in chronic myeloid leukemia that affects their adhesiveness, interaction with the microenvironment and resistance to imatinib (Chorzalska et al., Leukemia 2014). These phenotypic changes were caused by loss of Abelson interactor-1 (Abi-1) which regulates integrin α4 and the Src family kinases (SFKs) signaling pathways. To further delineate how organ-specific absence of Abi-1 affects hematopoiesis and hematopoietic stem cells, we generated a conditional, inducible bone marrow-specific Abi-1 transgenic mouse knockout model. For this purpose, we crossed conditional Abi-1(fl/fl) knockout mice with transgenic Tg(Mx1-cre+/-) mice (B6.Cg-Tg(Mx1-cre+ 1Cgn/J) that express Cre recombinase under the control of the polyinosinic:polycytidylic acid (poly(I:C)) or interferon-inducible Mx1 promoter. Obtained Abi-1(fl/fl);Tg(Mx1- cre(+)) animals were subjected to bone marrow-specific Abi-1 deletion induced by intraperitoneal administration of poly(I:C), resulting in organ-specific Abi-1 knockout (Abi-1 KO). Abi-1(fl/fl);Tg(Mx1- cre(-)) animals subjected to the same poly(I:C) treatment (Abi-1 WT) were used as controls in all experiments (Figure 1A). We confirmed the absence of Abi-1 protein in the Abi-1 KO bone marrow by immunoblotting (Figure 1B). Abi-1 KO mice developed deranged hematopoiesis with progressive anemia, thrombocythemia, megakaryocytosis, and myeloid hyperplasia (Figure 1C). They also developed progressive splenomegaly with 1.4x, 2.4x, and 4.8x enlargement of the spleen at 4, 28, and 50 weeks after recombination, respectively, and progressive femur pallor (Figure 1D) with bone marrow fibrosis confirmed by trichrome and silver staining (Figure 1D). Using fluorescence-activated cell sorting, we determined that Abi-1 KO resulted in more than two-fold expansion of the most primitive long-term hematopoietic stem cells (Lin-CD34-Sca-1+c-Kit+ CD135-) in the bone marrow and 3.75-fold increase of LSK cells (Lin- Sca-1+c-Kit+) in the peripheral blood compared with controls (Figure 1E). Increased activities of the SFKs and NFκB were observed in Abi-1 KO bone marrow, and confirmed in human CD34+ cells isolated from the marrow of patients with PMF or AML (Figure 1F,G). Furthermore, CD34+ hematopoietic progenitors and granulocytes from PMF patients, as well as CD34+ hematopoietic progenitors from AML patients, showed decreased levels of ABI1 transcript (Figure 1H).
Taken together, our results indicate that a targeted deactivation of Abi-1 in the bone marrow causes expansion of hematopoietic stem cells, myeloid hyperplasia with thrombocytosis and overproduction of collagen and reticulin fibers. The Abi-1 KO murine phenotype meets the Mouse Models of Human Cancers Consortium criteria for a myeloproliferative neoplasm with features resembling human PMF (Kogan et al., Blood 2002). These data indicate that loss of Abi-1 is sufficient for initiation of bone marrow fibrosis, and that Abi-1-SFKs-NFκB cross-talk may represent a new molecular target for the treatment of PMF.
Bone marrow-specific, conditional Abi-1 KO animals represent a new model of PMF offering a unique opportunity to interrogate the molecular details of the Abi-1-driven mechanism that leads to the development of stem cell-derived MPNs, and to elucidate potential novel therapeutic approaches that directly address their pathogenesis.
Olszewski:Bristol-Myers Squibb: Consultancy; Genentech: Research Funding; TG Therapeutics: Research Funding. Reagan:Alexion: Honoraria; Seattle Genetics: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal