Abstract
Allogeneic hematopoietic stem cell transplantation (aHSCT) is hampered by chronic graft-versus-host disease (cGVHD), which results in multi-organ fibrosis and loss of function. In particular, bronchiolitis obliterans (BO) and scleroderma resulting from fibrotic bronchiolar and cutaneous response, respectively, are two devastating outcomes for cGVHD patients. Fibrotic manifestations often are considered irreversible and progressive. Therefore, new therapies targeting fibrosis are urgently needed.
Pirfenidone (5-methyl-1-phenyl-2- (1H)-pyridone) exhibits a well-documented anti-inflammatory and anti-fibrosis function in multiple pre-clinical models and is the first and only FDA-approved drug for idiopathic pulmonary fibrosis. For this study, Pirfenidone was synthesized as a crystalline solid and found to be pure both by melting point and NMR spectroscopy. We evaluated Pirfenidone's anti-fibrosis function in 2 pathophysiologically distinct cGVHD murine models: 1. a major mismatched multi-organ system model (C57BL/6 to B10.BR) that induces BO as a result of a cGVHD-induced germinal center (GC) reaction, antibody deposition and fibrosis in the lung; and 2. a minor antigen mismatched model (B10.D2 to BALB/c) in which severe scleroderma is the major disease manifestation.
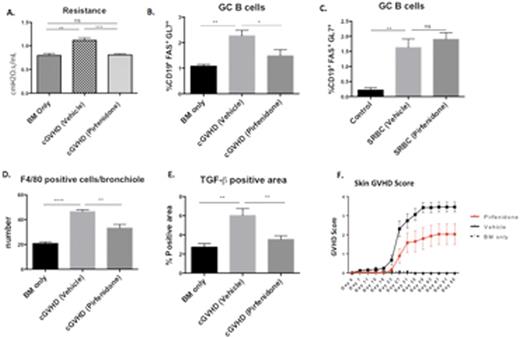
In the BO model, pulmonary function loss in cGVHD mice (as reflected by increased resistance, elastance and decreased compliance of the lung) was restored by Pirfenidone treatment (400mg/kg) during both the early (day28-56) (Fig A, representative of 3 experiments with 5-8 mice per group) and late stages (day56-84) of the disease. Pathologic changes in the lung, such as collagen deposition and narrowing of bronchioles, were significantly reduced by Pirfenidone. The size and frequency of GCs in the spleen, and the frequency of GC B cells (Fig B, representative of 2 experiments with 5-8 mice per group) and T follicular helper cells were all significantly reduced in Pirfenidone- treated groups. To determine whether GCs were directly affected by Pirfenidone, we evaluated Pirfenidone in C57BL/6 mice immunized with sheep red blood cells (SRBC) to induce GCs. Interestingly, Pirfenidone did not reduce the SRBC-induced GC reaction (Fig C) (comparable frequencies of splenic GC B cells, T follicular helper cells and serum IgG levels were seen between Pirfenidone and vehicle-treated groups). These results suggested that Pirfenidone suppresses the GC reaction through a cGVHD-specific mechanism, rather than through immune regulation. Mechanistically, Pirfenidone administration attenuated the sequestration of pro-fibrogenic F4/80+ macrophages (Fig D, representative of 2 experiments) and TGF-β (Fig E, representative of 2 experiments) production within the lung. These results have led us to elucidate a potential mechanism of cGVHD: antibody deposition in the lung results in the activation of macrophages and TGF-β that drive fibrotic change and tissue damage, resulting in the exposure of auto- and allo- antigens to the immune system that support and sustain pathologic GC reactions.
In the B10.D2 to BALB/c sclerodermatous cGVHD model, Pirfenidone treatment (400mg/kg, day21-55) improved clinical signs of scleroderma and reduced macrophage infiltration in the skin (Fig F).
In summary, this is the first study evaluating a commercially available anti-fibrosis drug on pathologically distinct pre-clinical cGVHD models. Our data suggests Prifenidone reversed cGVHD in the BO model and, to a lesser extent, in the scleroderma model. Thus, Pirfenidone is a novel therapeutic agent for treating cGVHD patients with fibrosis that have been typically refractory to therapies.
A. Resistance of lungs was measured on day56 of transplantation; Elastance and compliance correlated with resistance but were not shown here.
B. Flow cytometry analysis of GC B cells of no cGVHD vs cGVHD mice treated with Pirfenidone or vehicle;
C. Flow cytometry analysis of GC B cells from SRBC-immunized mice treated with Pirfenidone or vehicle;
D and E. Macrophage F4/80 and TGF-β quantification of day56 lungs of no cGVHD vs cGVHD mice treated as indicated;
F. Skin GVHD scores were recorded on indicated dates of irradiated BALB/c mice transplanted with B10.D2 donor BM alone or with T cells and treated as indicated. Unpaired student T test was used for statistical analysis. ****:P<0.0001; ***: P<0.001; **: P<0.01; *: P<0.05; ns: not significant.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal