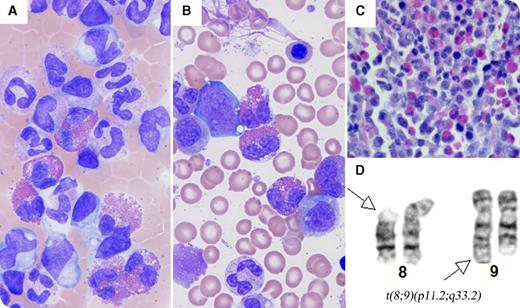
An 8-month-old male infant presented with a diffuse sandpaper-like rash, lymphadenopathy, hepatosplenomegaly, fever, tonsillar hypertrophy, frequent infections, and failure to thrive. Complete blood count showed marked leukocytosis (white blood cell count, 34.91 × 109/L; eosinophils, 23.9%; neutrophils, 43%; monocytes, 10.8%; lymphocytes, 18.5%; immature granulocytes, 3.8%) and anemia (hemoglobin, 7.9 g/dL). Peripheral blood smear revealed leukocytosis with markedly increased neutrophils, eosinophils, monocytes, and occasional immature granulocytes (panel A; Wright's stain, original magnification ×1000). Bone marrow showed myeloid hyperplasia with markedly increased eosinophils (11% of total nucleated cells) and 1% blasts (panels B-C; panel B, Wright-Giemsa stain, original magnification ×1000; panel C, hematoxylin and eosin stain, original magnification ×400). No infectious agent was identified. Cytogenetic analysis showed a 46,XY,t(8;9)(p11.2;q33.2) karyotype in 16 of 20 cells (panel D). Fluorescence in situ hybridization analysis showed FGFR1 rearrangement in 74% of cells. The patient underwent allogeneic unrelated bone marrow transplant and suffered graft-versus-host disease and multiple infections; he died at 19 months of age, 6 months after the transplant.
The differential diagnosis of eosinophilia is broad, and includes a variety of reactive conditions, infections, and malignancies. FGFR1-related myeloid neoplasms with eosinophilia are rare. This is the youngest patient reported in this category. This case highlights that myeloid neoplasms in any age group with unexplained eosinophilia, even without an increase in blasts, should be always considered and investigated with cytogenetics.
An 8-month-old male infant presented with a diffuse sandpaper-like rash, lymphadenopathy, hepatosplenomegaly, fever, tonsillar hypertrophy, frequent infections, and failure to thrive. Complete blood count showed marked leukocytosis (white blood cell count, 34.91 × 109/L; eosinophils, 23.9%; neutrophils, 43%; monocytes, 10.8%; lymphocytes, 18.5%; immature granulocytes, 3.8%) and anemia (hemoglobin, 7.9 g/dL). Peripheral blood smear revealed leukocytosis with markedly increased neutrophils, eosinophils, monocytes, and occasional immature granulocytes (panel A; Wright's stain, original magnification ×1000). Bone marrow showed myeloid hyperplasia with markedly increased eosinophils (11% of total nucleated cells) and 1% blasts (panels B-C; panel B, Wright-Giemsa stain, original magnification ×1000; panel C, hematoxylin and eosin stain, original magnification ×400). No infectious agent was identified. Cytogenetic analysis showed a 46,XY,t(8;9)(p11.2;q33.2) karyotype in 16 of 20 cells (panel D). Fluorescence in situ hybridization analysis showed FGFR1 rearrangement in 74% of cells. The patient underwent allogeneic unrelated bone marrow transplant and suffered graft-versus-host disease and multiple infections; he died at 19 months of age, 6 months after the transplant.
The differential diagnosis of eosinophilia is broad, and includes a variety of reactive conditions, infections, and malignancies. FGFR1-related myeloid neoplasms with eosinophilia are rare. This is the youngest patient reported in this category. This case highlights that myeloid neoplasms in any age group with unexplained eosinophilia, even without an increase in blasts, should be always considered and investigated with cytogenetics.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal