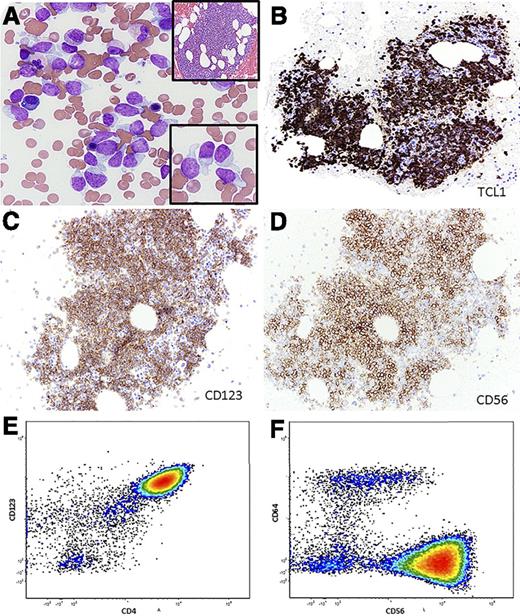
A 63-year-old man presented with cutaneous nodules. Workup revealed anemia, thrombocytopenia, monocytosis, and 5% circulating “blasts.” Bone marrow sampling showed 33% immature-appearing cells (panel A), with occasional “tadpole” appearance (panel A, lower inset) and an 80% cellular marrow with an interstitial infiltrate (panel A, upper inset). The neoplastic cells were positive for TCL1, CD123, and CD56 by immunohistochemistry (panels B-D). Flow cytometry demonstrated CD4, CD56, and CD123 expression (panels E-F), with absence of CD34 and lineage-specific markers. Cytogenetic analysis showed no clonal abnormalities, and next-generation sequencing showed 2 TET2 mutations (1 missense and 1 nonsense mutation: NM_001127208.2:c.3781C>T p.R1261C and c.2737C>T p.Q913*, respectively). A diagnosis of leukemic/disseminated blastic plasmacytoid dendritic cell neoplasm (BPDCN) was established. Biopsy of the cutaneous nodules confirmed involvement by BPDCN.
BPDCN is a rare neoplasm with poor prognosis. Acute myeloid leukemia (AML) has been reported in ∼20% of BPDCN patients and tends to arise metachronously. Distinguishing BPDCN from AML can be challenging. The tadpole or “hand mirror” appearance of the cells is helpful, but identifying the characteristic immunophenotype is essential in establishing the diagnosis. Recent data suggest that acute lymphoblastic leukemia-type regimens may be more effective compared to standard approaches using AML-type regimens in BPDCN. A therapeutic role may exist for agents targeting the nuclear factor κB pathway. An accurate diagnosis of BPDCN becomes more critical as targeted therapeutic options become available.
A 63-year-old man presented with cutaneous nodules. Workup revealed anemia, thrombocytopenia, monocytosis, and 5% circulating “blasts.” Bone marrow sampling showed 33% immature-appearing cells (panel A), with occasional “tadpole” appearance (panel A, lower inset) and an 80% cellular marrow with an interstitial infiltrate (panel A, upper inset). The neoplastic cells were positive for TCL1, CD123, and CD56 by immunohistochemistry (panels B-D). Flow cytometry demonstrated CD4, CD56, and CD123 expression (panels E-F), with absence of CD34 and lineage-specific markers. Cytogenetic analysis showed no clonal abnormalities, and next-generation sequencing showed 2 TET2 mutations (1 missense and 1 nonsense mutation: NM_001127208.2:c.3781C>T p.R1261C and c.2737C>T p.Q913*, respectively). A diagnosis of leukemic/disseminated blastic plasmacytoid dendritic cell neoplasm (BPDCN) was established. Biopsy of the cutaneous nodules confirmed involvement by BPDCN.
BPDCN is a rare neoplasm with poor prognosis. Acute myeloid leukemia (AML) has been reported in ∼20% of BPDCN patients and tends to arise metachronously. Distinguishing BPDCN from AML can be challenging. The tadpole or “hand mirror” appearance of the cells is helpful, but identifying the characteristic immunophenotype is essential in establishing the diagnosis. Recent data suggest that acute lymphoblastic leukemia-type regimens may be more effective compared to standard approaches using AML-type regimens in BPDCN. A therapeutic role may exist for agents targeting the nuclear factor κB pathway. An accurate diagnosis of BPDCN becomes more critical as targeted therapeutic options become available.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal