Hematopoietic stem cell transplant (HSCT) or solid organ transplant (SOT) recipients are often at high risk of developing Epstein-Barr virus (EBV)-associated lymphoproliferative disease (PTLD) due to underlying severe immunodeficiency.1,2 In particular, impairment of antiviral T-cell immunity as a result of immunosuppressive therapy is a critical risk factor for the development of PTLD.3 The impact of interaction between EBV with host B-cell subpopulations on the emergence of PTLD in transplant recipients has been a major area of interest for immunobiology experts. Understanding of these interactions may provide clues on how to control EBV-associated PTLD in transplant recipients. Early studies conducted by David Thorley-Lawson and colleagues first demonstrated that EBV persists in resting memory B cells in a nonpathogenic state with limited viral gene expression, which allows these cells to escape from antiviral T-cell control.4,5 Occasionally, these virus-infected memory B cells differentiate into plasma cells resulting in the activation of the EBV replicative cycle, which allows infection of more naïve B cells. In this issue of Blood, Burns et al have now extended these observations to provide an interesting insight into the biology of EBV infection in HSCT recipients, especially in the context of reconstitution of innate and adaptive immune cells.6
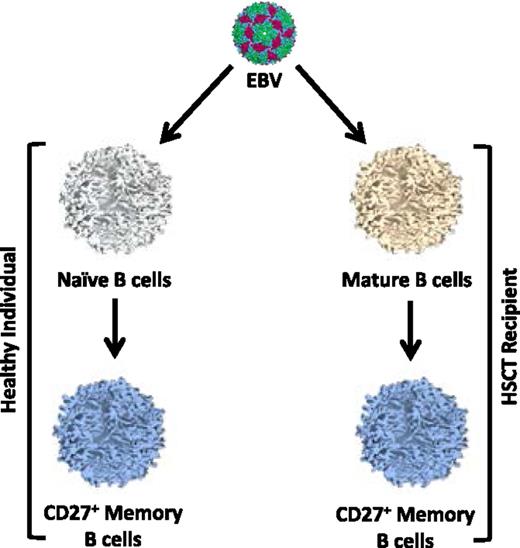
Alternative routes of EBV infection of B cells in immunocompetent and immunocompromised individuals. In healthy individuals, EBV-infected naïve B cells are driven to differentiate into memory cells within the germinal center. By contrast, HSCT recipients have poor germinal center responses for several months after transplant. Therefore, it is proposed that EBV either infects memory B cells present in the graft or newly emerging mature B cells that have recently differentiated from donor stem cells. In this latter scenario, it is unclear whether EBV infects naïve B cells and then drives them to differentiate into memory or directly infects rare memory B cells.
Alternative routes of EBV infection of B cells in immunocompetent and immunocompromised individuals. In healthy individuals, EBV-infected naïve B cells are driven to differentiate into memory cells within the germinal center. By contrast, HSCT recipients have poor germinal center responses for several months after transplant. Therefore, it is proposed that EBV either infects memory B cells present in the graft or newly emerging mature B cells that have recently differentiated from donor stem cells. In this latter scenario, it is unclear whether EBV infects naïve B cells and then drives them to differentiate into memory or directly infects rare memory B cells.
By prospectively monitoring EBV DNA in HSCT recipients, the authors of this study were able to identify patients who had high viral reactivation and others who had undetectable or low viral load. Follow-up analysis of these 2 groups of recipients revealed early emergence of CD27+ memory B cells in patients with high viral loads and selective infection of these cells with EBV. These CD27+ memory B cells express multiple latent transcripts including EBNA1, EBNA2, and LMP2 or LMP1 and also expressed the proliferation marker Ki-67. These observations raise an important question on how the pathway of EBV infection in HSCT recipients may be different from healthy virus carriers. As shown in the figure, EBV infection in immunocompetent individuals proceeds through the infection of naïve B cells, which is followed by migration to the germinal center where these cells differentiate into memory cells.7 Burns et al argue that this differentiation program is unlikely to operate in HSCT recipients as their normal germinal center activity is impaired due to the underlying deficiency of CD4+ T cells and other supporting cells. They propose that in the HSCT setting, either EBV infects donor mature memory B cells (transferred with engrafted cells) or newly emerging mature B cells that have differentiated from donor stem cells. Both these potential scenarios are consistent with the clinical evidence, but a formal proof will require further studies. More importantly, data presented by Burns et al provide an important platform for future design of immunotherapeutic strategies to prevent PTLD. Although anti-CD20 antibodies have emerged as gold standard therapy for PTLD, a novel design of bispecific antibodies targeting both CD20/CD19 and CD27 should be explored. This dual targeting in HSCT recipients with high viral load may prevent progression to PTLD.
Conflict-of-interest disclosure: The author declares no competing financial interests.