Abstract
Malignant lymphoma is a heterogenous group of diseases varied from pathological features, immunophenotypes and genetic characteristics. Although modern chemotherapy has remarkably improved the prognosis of the patients, targeted therapy on actionable tumor biomarkers, irrespective of pathological subtypes, remains great interests in lymphoma.
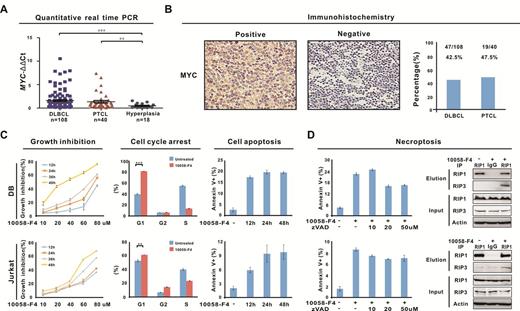
MYC was initially uncovered as the target of the t(8;14)(q24;q32) chromosome translocation in Burkitt lymphoma and subsequently identified as a master regulator in lymphoma progression. Here in patients with diffuse large B-cell lymphoma (DLBCL, n=108) and peripheral T-cell lymphoma (PTCL, n=40), MYC gene expression was significantly higher than that of reactive hyperplasia, in consistent with increased MYC protein expression (>40% by immunohistochemistry, Figure 1A-B). Moreover, pharmacological silencing of MYC using specific MYC inhibitor 10058-F4 induced B- and T-lymphoma cell growth inhibition, G0/G1 cell cycle arrest, apoptosis and necroptosis (Figure 1C-D). Therefore, MYC was overexpressed and biologically functional in main lymphoma subtypes like DLBCL and PTCL.
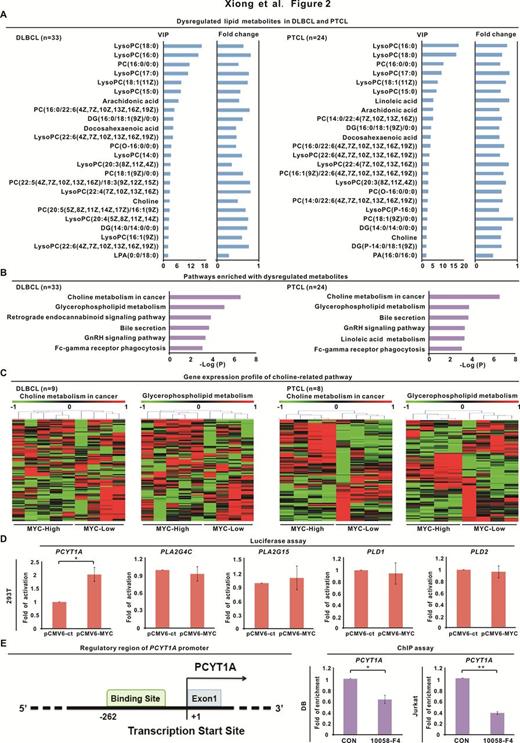
However, how to specifically target the unique dependencies of MYC-addicted malignant lymphocytes without influencing their normal counterparts warrants further investigation. Growing evidences showed that activation of oncogene reprograms tumor cell metabolism. Thus, serum metabolomic analysis was performed in 33 DLBCL patients, 24 PTCL patients and 50 healthy volunteers referred as the normal control. The results showed that dysregulation of choline metabolism occurred in both subtypes of lymphoma (Figure 2A-B). Importantly, using gene expression profile in frozen tissue samples of 9 DLBCL and 8 PTCL patients, distinct gene pattern of choline-related metabolic pathways was revealed according to MYC expression (Figure 2C). As mechanism of action, further luciferase and ChIP assay demonstrated that MYC modulated choline metabolism through transcriptionally activating choline-related enzyme phosphate cytidylyltransferase 1 choline alpha (PCYT1A) (Figure 2D-E).
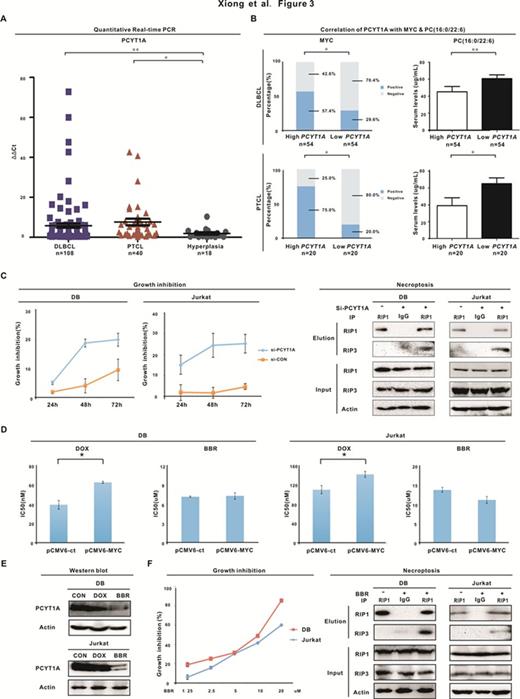
Increased expression of PCYT1A was observed in DLBCL and PTCL patients with higher tumor MYC expression, in accordingly with lower serum downstream choline metabolite phosphatidylcholine (Figure 3A-B) and International Prognostic Index indicating intermediate-high and high-risk. Meanwhile, molecular silencing of PCYT1A by siRNA inhibited lymphoma cell growth through inducing necroptotic cell death (Figure 3C). Lipid-lowering agent Berberine is an isoquinoline alkaloid isolated from several Chinese herbal medicines and exhibits anti-cancer effect in solid tumors. Interestingly, MYC-overexpressing lymphoma cells, resistant to chemotherapeutic agent doxorubicin, were sensitive to Berberine, which could downregulate PCYT1A expression, inhibit lymphoma cell growth and induce lymphoma cell necroptosis (Figure 3D-F).
Collectively, our data proved a direct link between MYC oncoprotein with aberrant choline metabolism in DLBCL and PTCL, highlighting the potential clinical utility of targeting MYC-dependent tumor cell metabolism in lymphoma. As a lipid-modifying enzyme, PCYT1A was controlled by MYC and attributed to dysregulation of choline metabolism. Functioned as a sensitive biomarker of lymphoma progression, PCYT1A could be targeted by lipid-lowering agent Berberine, providing a novel therapeutic strategy in treating MYC-driven lymphoma.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal