Abstract
Background: There remains a critical requirement for novel therapies for Acute Myeloid Leukemia (AML). Bromodomain and extra-terminal domain (BET) inhibitors are emerging as exciting therapeutic agents for hematopoietic malignancies. Pharmacological inhibition of BET bromodomains targets malignant cells by preventing reading of acetylated lysine residues, thus disrupting chromatin-mediated signal transduction, which reduces transcription at oncogenic loci. Although a heterogeneous disease, most AML retains wild type p53. However, p53 is often rendered functionally deficient by over-expression of MDM2. Potentiating the p53 response though MDM2 antagonism is therefore potentially beneficial to most AML subtypes. We hypothesized that dual inhibition of MDM2 and BET would be synthetic lethal to p53 wild type AML.
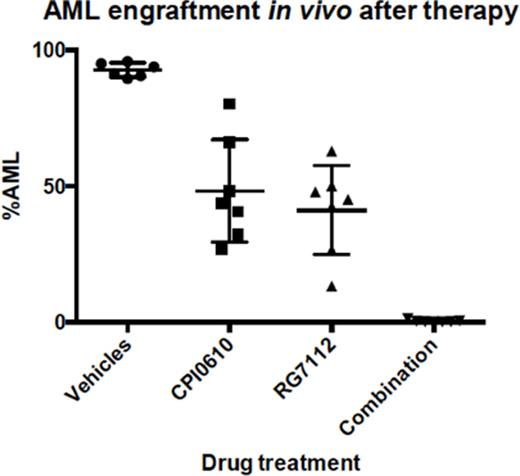
Methods: For in vitro experiments CPI203 (BET inhibitor, Constellation Pharmaceuticals) and nutlin-3 (MDM2 antagonist, Sigma) were assessed on p53 wild type cell lines (OCI-AML3, MOLM-13 and MV411) and p53 wild type primary murine AML. To assess the combination's dependency on wild type p53; p53 mutated cell lines (KG1a, KASUMI-1 and THP1) were tested. Cell viability was assessed using resazurin (Alamar blue dye) across numerous dose ratios on the OCI-AML3 cell line and analysed using the Envision Fluorescent Reader. Drug combination indices (CI) were evaluated using Calcusyn (version 2.0). Apoptosis was assessed using flow cytometry staining for Annexin V and propidium iodide (PI) on all p53 wild type and mutated cell lines. For in vivo experiments CPI0610 (clinical grade BET inhibitor, Constellation Pharmaceuticals) and RG7112 (MDM2 inhibitor, Roche) were tested as single agents, in combination and with relevant vehicle controls. RNA seq was performed on the GAIIX sequencer and gene ontology analysis was performed using DAVID/INGENUITY pathway analysis (IPA).
Results: In the OCI-AML3 cell line, resazurin analysis demonstrated that combining CPI203 with nutlin-3 was potently synergistic in decreasing viable cells for a 1:12.5 (mean CI=0.07) and 1:25 ratio (mean CI=0.299), and synergistic for a 1:50(mean CI=0.44) and 1:100(mean CI= 0.66) ratios. There was no benefit in using the combination treatment on the p53 mutated cell lines. Apoptosis was enhanced at least 1.5 fold (median 1.7, range 1.5-2.65) by the drug combination versus the single agents, in the panel of p53 wild type cell lines tested. Analysis of whole genome RNA seq on OCI-AML3 treated cells, showed that genes up-regulated by the combination of CPI203 and nutlin-3, had a thirty-fold enrichment for p53 signalling (FDR (<0.05). Down-regulated genes were enriched for FOXM1-dependent cell cycle progression genes.
To evaluate the combination in vivo, we used a Trib-2 driven primary AML where leukemogenesis is induced through inhibition of C/EBPα. Myeloblasts were transduced with GFP on the same retroviral construct asTrib-2 for disease tracking. Treatment was commenced in all mice (n=40), post confirmation of disease engraftment. Three mice from each treatment group were sacrificed after 48hrs and cells sorted for GFP to perform RNA seq in this in vivo setting. After 21 days of treatment all mice were sacrificed (n=27, one vehicle control succumbed to disease 15 days post engraftment). End of treatment results (primary read out was the GFP% which equates to the blast%) demonstrated superior in vivo efficacy of dual inhibition of MDM2 and BET in comparison with controls in eradicating AML, p<0.0001, (see figure). Importantly, normal haematopoiesis was spared - as evidenced by normal full blood counts and comparable myeloid, B-cell and T-cell populations with our C57bl6 wild type controls. RNA seq of the murine blasts revealed that many more genes significantly (FDR<0.05) changed expression in the combination treated mice than single agent treated mice. The p53 pathway was the most common up-stream regulator of genes changing expression post combination treatment, p<0.0001. The combination affected many more genes in the p53 pathway than RG7112 alone (120 genes versus 20 genes respectively), in line with our in vitro results.
Conclusion: This combination of BET and MDM2 inhibition is effective and superior to single agent therapy on all p53 wild type AMLs tested, in vitro and in vivo. In both contexts this is associated with potentiating the p53 response and could be relevant to many patients with p53 wild type AML.
Latif:Novartis: Honoraria. Copland:Ariad: Honoraria, Membership on an entity's Board of Directors or advisory committees; BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal