Abstract
Introduction: With the introduction of reduced-intensity conditioning (RIC), the age limit for allogeneic transplantation of AML patients has risen to 65 and above. In order to balance a low transplant-related mortality (TRM) with high anti-leukemic efficacy, Marks et al.1 introduced FBM conditioning consisting of 150mg/m2 Fludarabine, 300mg/m2 BCNU and 110mg/m2 Melphalan as RIC for elderly patients with encouraging results. However, no detailed analysis of factors predicting outcome in this subpopulation has been presented so far.
Methods: In this two-center retrospective study, 51 patients (pts) with a median age of 64 y (range, 44-75y) diagnosed with AML were uniformly treated according to the FBM protocol. GvHD prophylaxis consisted of Ciclosporin A (CYA) and mycophenolate mofetil (MMF) in all patients. MMF was tapered after d50 and CYA after d90 in the absence of GvHD. Pts with matched unrelated donors (MUD) (n=33) or mismatched unrelated donors (MMUD) (n=9) received additional ATG or low dose alemtuzumab as GvHD and rejection prophylaxis. 9 pts with matched related donor (MRD) only received CYA and MMF as GvHD prophylaxis. Stem cell source was peripheral blood in 90% (n=46) and marrow in 10% (n=5) of the patients. The median number of transfused CD34+ cell was 7.1 million per kg body weight. The median follow-up at the time of analysis was 27 months. At the time of transplant 38 pts were in complete remission; the rest of the pts had active disease (partial remission or refractory disease). Molecular (NPM1, FLT3-ITD and CEBPA a) and cytogenetic characteristics (evaluable in 50 patients) were available for all patients.
Results: Acute regimen-related toxicity was low, with a d30 mortality of 0 % in both centers. After 2 years, treatment failure was mainly due to relapse (CIR) with 36% (SE: 8%) in comparison to TRM (20%, SE: 7%). The resulting progression-free survival (PFS) and overall survival (OS) at 2 years was 50 % (SE: 5%) and 61% (SE: 7%), respectively.
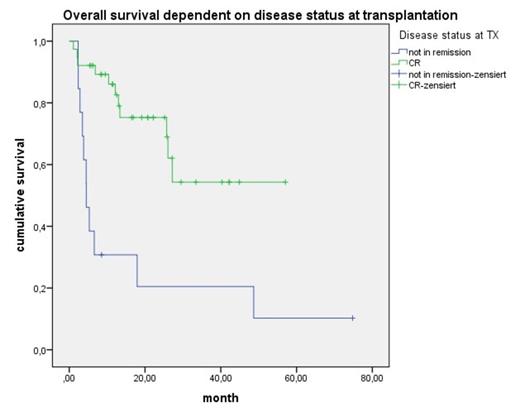
The median EBMT score was 4 (range 2-6). The EBMT score had no impact on different outcome variables (CIR (p=0.465), PFS (p=0.352) and OS (p=0.171)). Based on cytogenetic and molecular data patients were categorized according to the European LeukemiaNet (ELN) classification. 10% (n=5) of the patients belonged to the ELN favorable, 39% (n=20) to the ELN intermediate I, 29% (n=15) to the ELN intermediate II and 22% (n=11) to the ELN adverse risk group. Neither the ELN score itself nor stratification according to FLT3 -ITD or NPM1 mutation status or cytogenetic risk group impacted on outcome in our cohort. A trend for an improved OS in patients with NPM1 mutation (not stratified for FLT3-ITD or FLT3-TKD) was detected (p=0.255). By analyzing further risk factors such as remission status, donor type, age, CMV status, CD34+ cell number and acute or chronic GvHD we found the disease status at the time of transplant being the dominant predictor for OS. After 2 years patients transplanted not in remission had only an OS of 20% (SE: 8%) as compared to 75% (SE: 12%) in patients transplanted in CR (p<0.001) (Figure 1).
Conclusion: In this cohort of elderly patients with AML receiving allogeneic transplantation after FBM conditioning, disease status at the time of transplant was the dominant prognostic factor for outcome. At the present follow-up neither molecular status nor cytogenetics impacted OS, PFS or CIR, significantly. We conclude that alternative strategies have to be applied using FBM conditioning in refractory patients, i.e. the early tapering of immunosuppression and the use of donor lymphocytes or cytoreduction immediately before the start of conditioning. An additional focus should be on novel compounds, which might help to increase CR rates at time of transplant.
References
1. Marks R, Potthoff K, et al. Reduced-toxicity conditioning with fludarabine, BCNU, and melphalan in allogeneic hematopoietic cell transplantation: particular activity against advanced hematologic malignancies. Blood. 2008;112(2):415-425.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal