Abstract
BACKGROUND: Following induction chemotherapy for Acute Myeloid Leukemia (AML), patients in morphologic complete remission (mCR) with persistent cytogenetic abnormalities (PCA) have poor outcomes relative to those achieving a mCR without a PCA. Whether these patients have similar outcomes to those failing to achieve a mCR remains unknown. Furthermore, the reasons for the discordance between morphologic and cytogenetic findings have not been well described. To address these questions we conducted a retrospective review of AML patients treated at our centre.
METHODS: All non-Acute Promyelocytic Leukemia AML patients from 2004 - 2014 were eligible for inclusion however patients with normal cytogenetics at diagnosis, those not evaluated for remission and those lacking post-induction cytogenetics were excluded. mCR was determined by the attending hematopathologists after review of the bone marrow aspirate (BMA), the bone marrow trephine biopsy (BMTB) with or without immunohistochemistry and/or flow cytometry for the detection of residual disease particularly in equivocal cases.
RESULTS: Study criteria were met in 111 patients. Median age was 50 years (17.6 - 77) and 63% were males. Median white blood count at diagnosis was 5.5 x 109/L (0.4 - 307) and median BMB% was 56% (11 - 96%). Most (84%) had primary AML. Cytogenetics were favorable in 28%, intermediate in 41%, and unfavorable in 31% of the patients. Chemotherapy was anthracycline based in 88% and fludarabine based in 12% of patients.
Post-induction, 94 patients (85%) had mCR (78 CR + 16 CR with incomplete count recovery, CRi) following induction, 18 (19%) of whom had a PCA and thus discordance between morphologic and cytogenetic findings. There was no difference in the rate of discordance in those age ≤60 vs. age >60 (18.8 vs. 20%, p=1.0), in those with secondary AML vs. primary AML (36 vs. 16%, p=0.13) or in those treated with an anthracycline vs. fludarabine regimen (21 vs. 9%, p=0.68). Discordance was 0%, 28% and 27% in those with favorable, intermediate and unfavorable risk cytogenetics, respectively (p=0.002). A CRi was associated with higher rates of discordance relative to those in CR (50 vs. 12.8%, p=0.002).
When the effects of the quality of the BMA and BMTB on the rates of discordance was evaluated, higher rates of discordance were seen in patients with dilute BMA vs. those with non-dilute aspirates (75 vs. 16.7%, p=0.02) and in those with hypocellular BMTB vs. those with cellular/hypercellular/packed BMTB (43.8 vs. 14.7%, p=0.016). Patients with BMB% of >2% had higher rates of discordance vs. those with BMB% ≤2% (46 vs. 9%, p=0.0001)
No difference in discordance rates was observed between patients whose BMA were aparticulate/pauciparticulate vs. those with particulate samples (33.3 vs. 16.5%, p=0.15), in those whose BMA samples were hypocellular vs. those that were cellular/hypercellular (20 vs. 16.4%, p=0.67) and in those who had suboptimal BMTB vs. those who had adequate vs. good/excellent samples (25 vs. 18 vs. 20%, p=0.89). In multivariate analysis only the BMB% >2% was associated with high rates of discordance (p=0.0002, odds ratio = 26) between morphologic and cytogenetic findings.
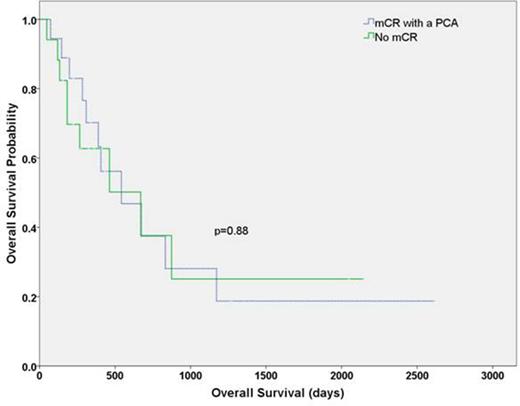
The outcomes of patients in mCR with a PCA (n=18) were compared with those failing to achieve a mCR (n=17). The two groups had similar characteristics although patients in mCR with a PCA had a lower median BMB% post-induction vs. those not in a mCR (3 vs. 6%, p=0.004). Of the 18 patients in mCR with a PCA, 10 (56%) underwent an allogeneic stem cell transplant (SCT) while 8 of the 17 (47%) patients not in mCR, after additional chemotherapy, went onto a SCT. Rate of relapse following SCT was similar for those with mCR with PCA vs. those not in mCR (62.5 vs. 33.3%, p=0.35) as was time to relapse (651 vs. 1973 days, p=0.56, Fig 1A). The median overall survival was also similar for patients with mCR and PCA relative to those not in mCR (542 vs. 670 days, p=0.88, Fig 1B).
Conclusions: Our results strongly reinforce the need to evaluate for persistent karyotype abnormalities post induction particularly amongst patients with BMB% >2%. Further prospective studies with larger cohorts are necessary to confirm our findings.
Overall survival. mCR, morphological complete remission; PCA, persistent cytogenetic abnormality.
Overall survival. mCR, morphological complete remission; PCA, persistent cytogenetic abnormality.
Sandhu:Celgene: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Janssen: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal