Abstract
Background: When administered subcutaneously (SC), the epigenetic modifier, azacitidine (AZA) is shown to improve overall survival in patients (pts) with AML compared with conventional care regimens (Fenaux, JCO, 2010; Dombret, Blood, 2015). CC-486, the oral formulation of AZA, is in clinical development for use in hematologic malignancies. An early dose-finding study of CC-486 administered on a 7-day schedule showed it to be safe and clinically active in pts with AML (Garcia-Manero, JCO, 2011; Gore, Blood, 2011). Extending CC-486 dosing for more than 7 days may increase AZA exposure to leukemic cells over the treatment (Tx) cycle to improve response.
Objective: Evaluate the safety and efficacy of CC-486 administered in extended dosing schedules (14 days or 21 days per 28-day cycle) in pts with AML.
Methods: Pts with AML from two phase I/II studies were sequentially assigned to receive CC-486 in 1 of 4 extended dosing regimens: 300mg QD x14 days (d)/28d (14-QD), 300mg QD x21d/28d (21-QD), 200mg BID x14d/28d (14-BID), or 200mg BID x21d/28d (21-BID). Hematologic responses (complete remission [CR], partial remission [PR], CR with incomplete hematologic recovery [CRi], marrow CR [mCR]), were assessed using IWG criteria for AML (Cheson, J Clin Oncol, 2003), and hematologic improvement (HI) and transfusion independence (TI) were assessed using IWG criteria for MDS (Cheson, Blood, 2006). Tx-emergent adverse events (TEAEs) were graded by NCI-CTCAE v3.1 or v4.0.
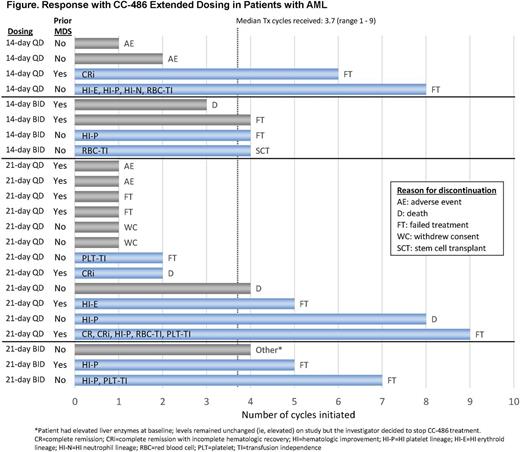
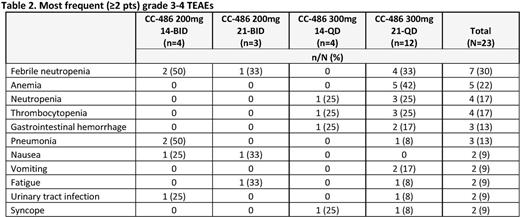
Results: In all, 23 pts with AML participated in the studies: 14-QD n=4, 21-QD n=12, 14-BID n=4, 21-BID n=3. Median age was 68 years (range 44 - 93), 48% were male, 22% and 78% had ECOG performance status scores of 0-1 or 2, respectively, median % bone marrow blasts was 25%, and median baseline hematology counts were: Hgb 9.1 g/dL (7.4 - 11.7), platelets 33 x 109/L (3 - 435), and ANC 0.3 x 109/L (0 - 6.4). Median time from diagnosis was 1.1 month (range -0.2 - 82.1). Eleven pts (52%) had prior MDS and 13 pts (57%) had received prior Tx for MDS (n=5) or AML (n=8), including 5 pts (38%) who had received hypomethylating agents (HMAs). The median number of CC-486 Tx cycles for all pts was 4 (1 - 9) (Figure). Overall response (CR, PR, CRi, mCR, HI or TI) rate was 48% (11/23), with generally comparable responses and response rates across the 4 dosing regimens (Table 1). Responses were observed in 4 pts (50%) who were relapsed/refractory to prior AML Tx. Two pts (40%) who had received prior HMA Tx responded, 1 of whom attained CR. HI was achieved by 32% (7/22) of pts, and 20% (3/15) of RBC transfusion-dependent pts attained RBC TI. Six pts with prior MDS (55%) responded during Tx. One pt proceeded to transplant. Febrile neutropenia (30%) and anemia (22%) were the most common grade 3-4 TEAEs (Table 2). Incidences of grade 3-4 TEAEs were generally similar across the 4 CC-486 dosing regimens.
Conclusions: CC-486 administered in extended 14- or 21-day per cycle schedules was well tolerated. One-half of these older pts with AML had a hematologic response, including pts who had prior MDS, or AML that failed or lost response to prior Tx. Interestingly, pts who previously received injectable HMA Tx had hematologic responses (including CR) with CC-486, likely due to the alternative methylation pattern obtained with prolonged oral administration (Laille, Plos One, in press). Ease of administration of CC-486 can facilitate long-term Tx for sustained disease modification, provide an additional option for failure of IV/SQ HMA therapy, and may improve outcomes in combination Tx regimens, which warrant investigation.
Savona:Karyopharm: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees; Gilead: Membership on an entity's Board of Directors or advisory committees; Incyte: Membership on an entity's Board of Directors or advisory committees, Research Funding. Gore:Celgene: Consultancy, Honoraria, Research Funding. Kolibaba:Janssen: Research Funding; Acerta: Research Funding; Amgen: Research Funding; Celgene: Research Funding; Gilead: Consultancy, Research Funding; Pharmacyclics: Research Funding; TG Therapeutics: Research Funding; Cell therapeutics: Research Funding; GSK: Research Funding; Novartis: Research Funding; Genentech, Inc.: Research Funding; Seattle Genetics: Research Funding. Ukrainskyj:Celgene Corporation: Employment, Equity Ownership. Kumar:Celgene Corporation: Employment, Equity Ownership. Dong:Celgene Corporation: Employment, Equity Ownership. Hetzer:Celgene Corporation: Employment, Equity Ownership. Skikne:Celgene Corporation: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal