Abstract

Introduction
Allogeneic hematopoietic stem cell transplant (allo-SCT) is the only curative treatment modality for patients with CMML. Here we retrospectively reviewed the data for patients with CMML who received an all-SCT at our institution to identify factors associated with improved survival and determine whether treatment with hypomethylating agents (HMA) before transplant improves survival for these patients.
Methods
All 83 patients 18 years of age or older with a diagnosis of CMML confirmed at The University of Texas MD Anderson Cancer Center who underwent allo-SCT between April 1991 and December 2013 were identified through review of the institutionÕs medical records and included in this analysis. Forty, 7, and 36 patients had CMML-1, CMML-2 and CMML that had progressed to AML (CMML/AML) respectively.
The median age was 57 years. CMML specific cytogenetic risk at diagnosis (Such E, hematologica, 2011) was good, intermediate, and high risk in 46, 19, and 18 patients respectively. Seventy-eight patients received induction treatment before transplant, 37 receiving HMA (either 5-azacytidine or decitabine) for at least 3 courses and 41 receiving 1-2 courses of cytotoxic chemotherapy. Among the patients who received induction therapy, 15 patients in HMA group and 9 patients in convention chemotherapy group achieved a complete remission before transplant.
Thirty, 47 and 6 patients received transplants from matched related donors (MRD), matched unrelated donors (MUD), and mismatched related or unrelated donors (MMD), respectively. The sources of hematopoietic stem cells were peripheral blood for 48 patients (57.8%) and bone marrow for 35 patients (42.2%). Conditioning regimens varied; most patients received either fludarabine in combination with busulfan or fludarabine combined with melphalan. Sixty-four patients received myeloablative and 19 patients received reduced intensity conditioning regimens. Graft-versus-host disease (GVHD) prophylaxis consisted of tacrolimus and methotrexate.
Patient and transplant characteristics did not significantly differ between the patients treated with HMA and the patients treated with conventional chemotherapy or given supportive care alone.
The primary endpoint was progression-free survival (PFS). The secondary endpoints were overall survival (OS), Treatment related mortality (TRM), relapse incidence through last follow-up and incidences of acute GVHD and chronic GVHD. All of these outcomes were measured from the time of allo-SCT.
Results
Median follow up duration for 29 survivors was 48 months. Seventy-five patients engrafted (90.4%) with median time to neutrophil and platelet engraftment of 13 and 15 days respectively.
Patients treated with a HMA had a significantly lower cumulative incidence (CI) of relapse at 3 years post-transplant (22%) than those treated with other agents (35%; p=0.03), whereas TRM at 1 year post-transplantdid not significantly differ between the groups (27% and 30%, respectively; p=0.84). Acute GVHD all grades and grade 2-4 were seen in 28.2% versus 35.8% (p=0.05) and 12.8% versus 11.3% (p=0.72) in patients who received a HMA compared to those who treated with other agents respectively. CI of chronic GVHD was 35% in patients treated with a HMA versus 19.2% in those treated with other agents (p=0.36) while CI of chronic extensive GVHD was seen in only 26.7% versus 19.2% respectively (p=0.64).
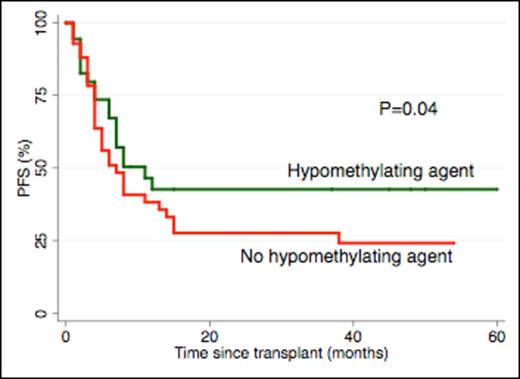
The lower relapse rate resulted in a significantly higher 3-year PFS rate in patients treated with a HMA (43%) than in those who received other treatments (27%; p=0.04) (Figure 1). However, therapy with HMA before transplant did not significantly influence the 3-year OS rate (45% in those treated with HMA and 39% in those treated with other agents; p=0.22).
The independent prognostic factors for PFS were a blast count of < 5% before transplant (HR 0.36, 95%CI 0.14-0.78), treatment with a HMA (HR 0.44, 95% CI 0.23-0.86), a transplant from an MRD (HR 0.41, 95% CI 0.22-0.94), development of grade 2-4 acute GVHD (HR 2.7, 95% CI 1.27-5.77), and development of chronic GVHD (HR 0.15, 95% CI 0.05-0.45).
Conclusion
We conclude that treatment with hypomethylating agents before allo-SCT may improve survival in patients with CMML.
Progression free survival
Alousi:Therakos, Inc: Research Funding. Andersson:Otsuka Research and Development, Inc.: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal