Abstract

Allogeneic hematopoietic cell transplantation (HCT) is considered definitive consolidation therapy for many patients with acute myeloid leukemia (AML) once complete remission (CR) is achieved. Nevertheless, relapse remains a major cause of treatment failure post-HCT.Increasing evidence suggests that the presence of minimal residual disease (MRD) at the time of HCT identifies a subset of patients that is at high risk of relapse.
In the present analyses, we sought to determine the impact of MRD detected by 8-color flow cytometry (FC) at HCT on 1-year relapse incidence (RI) in patients transplanted in first CR (CR1).
Between 2010 and 2012, 159 AML CR1 patients with a median age of 53 years were transplanted with matched sibling donor (MSD, n=42), matched unrelated donor (MUD, n=78) or mismatched donor (MMD (n=39). Of 159 patients, 50 had MRD by 10-color FC at HCT (MRDpos). Compared with patients without MRD (MRDneg), MRDpos were older (median age 60 vs. 53, p=0.0003), required more than 1 line of induction chemotherapy to achieve CR1 (40% vs. 17%, p=0.001), had more incomplete recovery of counts (CRi/p) at HCT (58% vs. 9%, p<0.001) and had more complex karyotype (CK) as diagnostic abnormality (25% vs. 13%, p=0.08). The distribution of conditioning intensity and donor type were similar between groups.
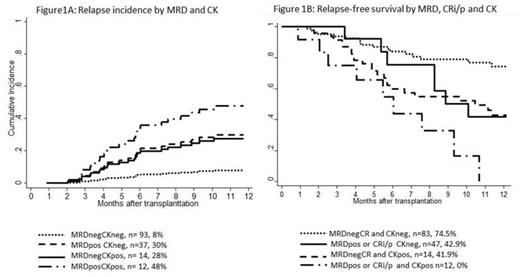
The median follow-up of 105 survivorswas 368 days. MRDpos patients had a higher 1-year RI (HR=3.2, p=0.003) compared with MRDneg,. Patients with CK was another group with higher 1-year RI compared with patients without CK (HR=3.2, p=0.003). Multivariate regressions showed that MRDnegCKneg patients represented the best prognostic group with the lowest 1-year RI while MRDposCKpos was the worst prognostic group (HR=6.8, p=0.002). Patients with either MRDpos or CKpos represented an intermediate risk group (HR=3.2, p=0.03) for 1-year RI after HCT (Figure 1a). The 1-year RI adjusted by age, line of induction regimen to achieve CR, intensity and donor type was 8% for MRDnegCKneg, 30% for MRDposCKneg and 47% for MRDposCKpos patients.
Similarly, 1-year relapse-free survival (RFS) was lower for patients who were MRDpos (HR=1.9, p=0.01) compared with patients who were MRDneg. Among other variables, CRi/p (HR=2.0, p=0.01) and CK (HR=2.2, p=0.009) also decreased 1-year RFS. Multivariate regressions showed that patients with MRDnegCKneg with complete count recovery at HCT had the best 1-year RFS and CKpos patients with either MRDpos or CRi/p had the worst outcomes (HR=5.2, p<0.001). Patients with only CKpos (HR=2.4, p=0.048) and CKneg but either MRDpos or CRi/p (HR=2.7, p=0.002) represented an intermediate risk group for 1-year RFS (Figure 1b).
Our study shows that MRD by FC at HCT is associated with other high risk disease features and its prognostic impact on 1-year RI is not independent of the cytogenetic risk profile. Patients without CK enjoy a lower incidence of relapse with better RFS even if they are MRDpos at HSCT. We believe that this group of patients with CKpos and MRDpos or CRi/p should be a target of innovative transplant and post-transplant strategies to further improve their outcomes.
Demographic by MRD
| . | MRDneg . | MRDpos . | P . |
|---|---|---|---|
| Median age | 53 | 60 | <0.001 |
| AML-t | 18 (17%) | 11 (22%) | 0.4 |
| CRi/p | 10 (9%) | 29 (58%) | 0.1 |
| Complex karyotype | 14 (13%) | 12 (25%) | 0.08 |
| ≥2 lines of induction to achieve CR1 | 18 (17%) | 20 (40%) | 0.001 |
| Myeloablative conditioning | 66 (61%) | 26 (52%) | 0.3 |
| MUD/MMD | 53/26 (49%/24%)) | 25/13 (50%/26%) | 0.8 |
| . | MRDneg . | MRDpos . | P . |
|---|---|---|---|
| Median age | 53 | 60 | <0.001 |
| AML-t | 18 (17%) | 11 (22%) | 0.4 |
| CRi/p | 10 (9%) | 29 (58%) | 0.1 |
| Complex karyotype | 14 (13%) | 12 (25%) | 0.08 |
| ≥2 lines of induction to achieve CR1 | 18 (17%) | 20 (40%) | 0.001 |
| Myeloablative conditioning | 66 (61%) | 26 (52%) | 0.3 |
| MUD/MMD | 53/26 (49%/24%)) | 25/13 (50%/26%) | 0.8 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal