Abstract
We conducted a multicenter study to evaluate a new enumeration method of hematopoietic progenitor cells (HPC) using an automated hematology analyzer, the XN-series model (Sysmex Corporation, Japan). This method appeared to be very promising in a pilot study in a single institution [Tanosaki R, et al. Int J Lab Hematol 2013]. We herein discuss the final results of our study.
PB or PBSC samples were taken from G-CSF- and/or chemo-mobilized subjects. The samples were divided into two tubes, one for an in-house assay where HPC were counted in each institution and one was shipped to a central laboratory (SRL, Inc., Japan) where the CD34+ cell count was examined. Firstly, we examined the frequency of invalid data. Secondly, the correlation between HPC and CD34+ cells was investigated. Thirdly, cut-off HPC values were determined to predict certain CD34+ cell counts, i.e. 20 cells/µL for PB and 1,000 cells/µL for PBSC. Finally, for the clinical application, we estimated values which predicted more than certain CD34+ cell counts with 95% probability by constructing a two-dimensional normal distribution model. This study was approved by the IRB of each institution, and informed consent was obtained from each participant before apheresis.
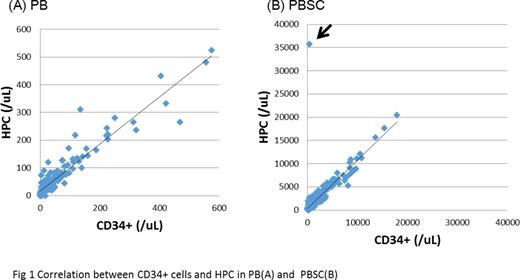
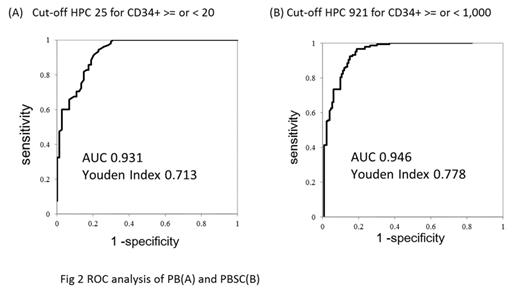
One hundred and nine subjects (46 healthy donors and 63 patients undergoing PBSCT) were registered in 5 institutions, and 954 HPC measurements from 614 samples were performed. Thirteen (4.4%) HPC values in 297 PBSC assays were estimated to be invalid, which was identified by an asterisk automatically applied to the corresponding result. Next, the data of the first assay from each sample where both the HPC and the central laboratory-based CD34+ count were available were extracted, and 470 HPC-CD34+ pairs from 102 subjects (43 healthy donors and 59 patients) were used for further analyses. The median age was 50.5 years (range, 3-78), 60 males and 42 females, and diagnoses were malignant lymphoma 28 patients, multiple myeloma 27, and others. It was revealed that there was one mismatched result in the PBSC samples (arrow in Fig 1B; HPC 35,768/µL, CD34+ 399/µL). When this value was removed, strong correlations between the HPC and CD34+ cell counts were observed in both the PB (r=0.94) and PBSC (r=0.97) samples (Fig 1). Strong correlations were observed also at each institution. The HPC cut-off values to distinguish CD34+ cell counts below or above 20/µL in PB and 1,000/µL in PBSC samples were determined to be 25 (AUC 0.931, Youden Index 0.713) and 921 (AUC 0.946, Youden Index 0.778), respectively, by a ROC analysis (Fig 2). Finally, HPC of 56/µL was determined to be the optimal value for predicting more than 20/µL of CD34+ cells in the PB samples with 95% probability.
This study confirmed that there was a strong correlation between the HPC and CD34+ cell count in a larger number of patients with different diagnosis at different institutions. For the PBSC collection, HPC ≥ 25/µL suggested an appropriate timing, and HPC 56/µL indicated a more secure threshold. HPC may also be a useful marker to rapidly estimate the quantity of CD34+ cells in the apheresis product. In cases where the HPC value is invalid, this may be overcome by serially evaluating HPC in the clinical course. In conclusion, HPC may be a good surrogate or an alternative for the CD34+ cell count. Prospective studies are warranted to verify the usefulness of HPC in clinical practice.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal