Abstract

Background
Long-term outcomes from autologous stem cell transplant (ASCT) in patients (pts) with relapsed/refractory (R/R) Hodgkin lymphoma (HL) are significantly better in patients who achieve a complete remission (CR) from salvage chemotherapy prior to ASCT. However, standard salvage therapy produces variable CR rates (19%-60%) and is associated with significant toxicity. Brentuximab vedotin and bendamustine are highly active when administered as single agents to pts with R/R HL (34% and 33% CR rates, respectively) and have manageable safety profiles. This phase 1/2, single-arm, 2-stage, open-label study was designed to evaluate the safety and efficacy of brentuximab vedotin in combination with bendamustine for the treatment of pts with primary refractory disease or in first relapse (ClinicalTrials.gov #NCT01874054).
Methods
Pts received an outpatient IV infusion of 1.8 mg/kg brentuximab vedotin on Day 1 with bendamustine on Days 1 and 2 of 3-week cycles for up to 6 cycles. Pts could undergo ASCT any time after Cycle 2 and post-transplant resume treatment with brentuximab vedotin as monotherapy for up to 16 total doses. Phase 1 was designed to determine the recommended dose of bendamustine, with an initial dose of 90 mg/m2 and a de-escalation scheme to be implemented if it exceeded the maximum tolerated dose. During phase 2, bendamustine was administered at the recommended dose in order to assess the CR rate of the combination. Response was assessed by the investigator per Cheson 2007. Enrollment is complete and long-term follow-up for PFS and OS continues.
Results
Fifty-five pts (56% female) with a median age of 36 yrs (range, 19-79) were enrolled. Fifty-one percent of pts had relapsed disease and 49% of pts had primary refractory disease after frontline therapy. A median of 13.8 mos (range, 3-98) had elapsed since initial diagnosis.
No dose-limiting toxicities were observed in the safety cohort, thus the recommended dose of bendamustine in combination with brentuximab vedotin was 90 mg/m2. Pts received a median of 2 cycles (range, 1-6) of the combination and a median of 9 cycles (range, 1-14) of single-agent brentuximab vedotin.
The main toxicity observed with the combination was infusion-related reactions (56% overall). The most common symptoms (≥10%) were pyrexia (26%), chills (20%), dyspnea and nausea (15% each), flushing (13%), and hypotension (11%). Premedication with corticosteroids and antihistamines was instituted with a protocol amendment and appeared effective. Before the amendment, 6 pts (24% of treated pts) discontinued treatment prematurely because of IRRs; post-amendment, IRRs led to treatment discontinuation for 2 pts (7%).
The CR rate of the combination was 74% (39/53 pts evaluable for response) and the overall objective response rate (CR and partial remission) was 93% (49/53 pts). The CR rate was 64% and 84% for refractory and relapsed pts, respectively.
Stem cell collection after first-line mobilization (G-CSF± plerixafor) was successful in 93% of pts (37/40). Median number of CD34+ cells collected was 4.1 x106 (Q1, Q3: 3.0, 5.4) in a median of 2 (range, 1-5) apheresis sessions. Median time to neutrophil and platelet engraftment was 11 days (range, 9-21) and 13 days (range, 9-39), respectively.
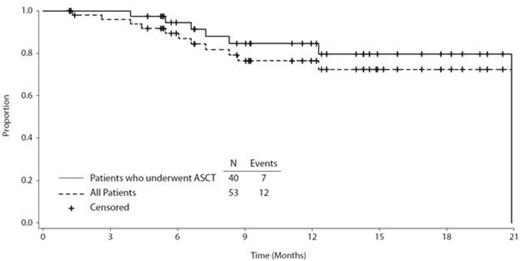
Pts have been followed for a median of approximately 1 year from first dose (median = 418 days; range, 118-635) and approximately 10 mos (314 days; range, 13-553) from ASCT. To date, 12 progression events have been observed: 7 in the 40 pts who underwent transplant and 5 in the 13 pts who did not undergo transplant. The estimated 12-mos PFS is 80% for both the transplanted population (95% CI: 70%, 90%) and the overall population (95% CI: 60%, 90%). Three of the 12 progression events were deaths; 2 pts died from progression of their HL and 1 pt died from septic shock after transplant.
Conclusions
The outpatient regimen of brentuximab vedotin 1.8 mg/kg on Day 1 in combination with bendamustine 90 mg/m2 on Days 1 and 2 of 3-week cycles induced a very high CR rate that compares favorably with historical data. The regimen has a manageable safety profile, with the most significant side effect being IRRs that can be successfully managed by premedication. The estimated 12-mos PFS rate of 80% demonstrates response durability, making the combination a promising salvage regimen for pts with HL in the first relapse setting.
Progression-Free Survival
Off Label Use: Brentuximab vedotin is indicated in the US for treatment of patients with Hodgkin lymphoma after failure of autologous stem cell transplant or after failure of at least two prior multi-agent chemotherapy regimens in patients who are not ASCT candidates and for the treatment of patients with systemic anaplastic large cell lymphoma after failure of at least one prior multi-agent chemotherapy regimen. This study evaluates brentuximab vedotin in HL patients with primary refractory disease or in first relapse. . Sawas:Seattle Genetics, Inc.: Research Funding. Agura:Seattle Genetics, Inc.: Research Funding. Matous:Takeda Pharmaceuticals International Co.: Speakers Bureau; Celgene: Consultancy, Speakers Bureau; Seattle Genetics, Inc.: Research Funding, Speakers Bureau. Ansell:Bristol-Myers Squibb: Research Funding; Celldex: Research Funding. Crosswell:KIYATEC (employment); Gilead (common stock ownership and research funding): Employment, Equity Ownership, Research Funding. Islas-Ohlmayer:Seattle Genetics, Inc.: Research Funding. Behler:Seattle Genetics, Inc.: Research Funding; Onyx Pharmaceuticals: Speakers Bureau. Cheung:Seattle Genetics, Inc.: Research Funding. Forero-Torres:Seattle Genetics, Inc.: Research Funding. Vose:Seattle Genetics, Inc.: Honoraria, Research Funding. Josephson:Seattle Genetics, Inc.: Employment, Equity Ownership. Advani:Seattle Genetics, Inc.: Research Funding; Genetech: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal