Abstract
Background: In primary myelofibrosis (PMF), ̴ 88% of patients harbor one of three "driver" mutations, with mutational frequencies of approximately 60%, 22% and 6% for JAK2, CALR and MPL, respectively. Other "non-driver" mutations have also been described in PMF and some of them and their number have been associated with inferior survival (Leukemia. 2014;28:1804). We applied next generation sequencing (NGS) with a broader panel of MPN-relevant genes, in order to identify additional mutations of prognostic relevance as well as obtain additional information regarding the prognostic value of 'number of mutations'.
Methods: Targeted capture assays were carried out on bone marrow or whole blood DNA specimens obtained at time of referral for the following genes: TET2, DNMT3A, IDH1, IDH2, ASXL1, EZH2, SUZ12, SRSF2, SF3B1, ZRSR2, U2AF1, PTPN11, Tp53, SH2B3, RUNX1, CBL, NRAS, JAK2, CSF3R, FLT3, KIT, CALR, MPL, NPM1, CEBPA, IKZF, and SETBP1. Paired-end indexed libraries were prepared from individual patient DNA using the NEB Next Ultra Library prep protocol on the Agilent Bravo liquid handler (NEB, Ipswich, MA/Agilent Technologies Inc, Santa Clara, CA). Capture libraries were assembled according to Nimblegen standard library protocol (Roche Nimblegen, Inc, Basel, Switzerland). Base-calling was performed using Illumina's RTA version 1.17.21.3. Genesifter® software was utilized (PerkinElmer, Danvers, Massachusetts) to analyze targeted sequence data. Nucleotide variants were called using the Genome Analysis Toolkit (GATK-Broad Institute, Cambridge, MA). Specific variants were deemed as mutations if they are associated with a hematologic malignancy (as identified by COSMIC database), or if they have not been associated with a dbSNP.
Results: 180 PMF patients were evaluated (median age 63 years; 65% males). DIPSS-plus risk distribution was 32% high, 38% intermediate-2, 17% intermediate-1 and 13% low. Driver mutation distribution was 62% JAK2, 22% CALR, 9% triple-negative and 7% MPL. Karyotype was abnormal in 41% of patients and unfavorable in 12%.
Mutations other than JAK2, CALR or MPL (i.e. "non-driver" mutations) were seen in 150 (83%) patients including 88% of "triple-negative" cases. 62 (34%) patients harbored one, 55 (31%) two, 16 (9%) three and 17 (10%) four or more. Mutational frequencies were: ASXL1 36%, TET2 18%, SRSF2 17%, U2AF1 17%, ZRSR2 11%, SF3B1 10%, DNMT3A 9%, CEBPA (9%), Tp53 7%, SETBP1 6%, CBL 5%, IDH1/2 5%, SH2B3 4%, CSF3R 4%, NRAS 4%, RUNX1 3% and ≤2% for SUZ12, KIT, PTPN11, NPM1 and EZH2. DIPSS-plus high/intermediate-2 risk patients displayed higher number of mutations (p=0.0004) and higher mutational frequencies for ASXL1 (p=0.02), SRSF2 (p=0.004) and CBL (p=0.02). Associations noted included JAK2 with U2AF1 (p=0.03), unfavorable karyotype with CBL (p=0.01) and normal karyotype with ZRSR2 mutations (p=0.04).
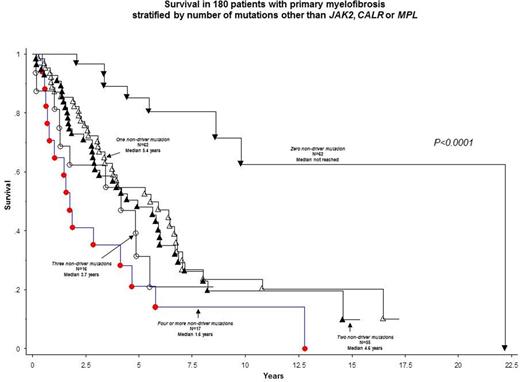
At a median follow-up of 4 years, 111 (62%) deaths were documented. For examination of impact on survival, we considered 'number of mutations' and specific mutations with >2% frequency. Accordingly, in univariate analysis, survival was adversely affected by 'number of mutations' (Figure 1) and presence of ASXL1, SRSF2, IDH1/2, U2AF1, RUNX1 and CBL mutations. For multivariable analysis, we considered three categories (zero, 1-3 and ≥4) for number of mutations based on the results from univariate analysis (Figure 1); the results showed ≥4 mutations, 1-3 mutations, RUNX1, CBL, ASXL1 and SRSF2 mutations were independently associated with shortened survival; the respective HR (95% CI) were 4 (1.4-11.1), 3 (1.3-6.8), 2.9 (1.1-8.1), 2.8 (1.3-6.3), 1.8 (1.2-2.7) AND 1.7 (1.03-2.7). When the multivariable analysis was repeated including only the 150 patients with at least one non-driver mutation, the 'number of mutations' was no longer significant (p=0.35) but ASXL1, CBL, RUNX1 and SRSF2 mutations retained their significance. The prognostic relevance of ASXL1 and CBL continued to be apparent even after the addition of DIPSS-plus and driver mutation profile to the multivariable model.
Conclusions: Mutations other than JAK2, CALR or MPL occur in more than 80% of patients with PMF, including those with "triple-negative" driver mutational status. The absence of such mutations is independently favorable for survival while the prognostic effect of their presence is influenced by ASXL1, CBL, RUNX1 and SRSF2 mutations.
Pardanani:Stemline: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal