Abstract
Follicular lymphoma (FL) is an indolent B-cell neoplasm of germinal center origin. Standard treatment regimens consist of anti-CD20 therapy with or without chemotherapy and while high response rates are common, relapses and progression ultimately occur. Alliance (formerly CALGB) has been testing rituximab-based biologic therapies in a series of phase 2 trials for previously untreated (CALGB 50901, 50402, 50701, 50803) or recurrent (CALGB 50401) FL. Clinical risk factors such as the FL international prognostic index (FLIPI) have been identified but there is need for prognostic and predictive biomarkers. In this exploratory analysis, we studied a series of immunohistochemical (IHC) markers of lymphoma cells (CD10, BCL2, BCL6, MUM1, Ki67) and the microenvironment (CD68, cytotoxic T cells, Tregs, Tfh) using tissue microarrays (TMAs) and correlated them with study endpoints to define markers of interest for future phase 3 trials.
FL diagnosis and grade were histologically confirmed by central review. Grade 3b cases were excluded. TMAs were constructed from 1mm diameter formalin-fixed paraffin-embedded tissue cores. IHC stains were performed using standard laboratory methods. The following stains were scored as follows by 3 hematopathologists via consensus review: Blimp1 - >5% positive; follicular (F)-BCL2 - >20% positive; F and interfollicular (IF)-CD10, F and IF-BCL6 - positive vs negative; MUM1, FoxP1, F and IF-PD1, granzyme B - % cells positive; FoxP3 - F, perifollicular or diffuse staining pattern; and CD68+ macrophages - # positive cells/high power field (hpf). Ki67 proliferation index (% positive cells) was evaluated using image analysis software (Definiens, Carlsbad, CA). Results were correlated with response to therapy and progression-free survival (PFS). Associations with response were measured using chi-square analysis. PFS was estimated using the Kaplan-Meier method and differences in PFS were compared using the log-rank test.
Patients in the 4 trials of untreated FL (N=241) were analyzed in aggregate for the purposes of biomarker analysis, and included 124 men and 117 women (median age 56 yrs). All had stage III, IV, or bulky stage II (single mass ≥7cm in any dimension) disease. By FLIPI, 58 (25%) had low-risk, 134 (57%) had intermediate-risk and 44 (19%) had high-risk disease. CALGB 50901 patients were slightly older with a greater proportion of intermediate-risk disease. CALGB 50803 patients had significantly better response and PFS.
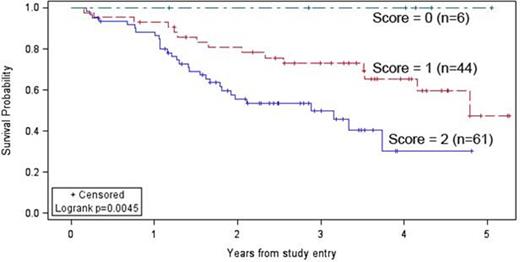
Among patients with available tissue, IF-CD10 positivity was seen in 79/127 (62%) and was associated with shorter PFS compared to IF-CD10-negative cases (2 yr PFS: 59% vs 80%, p=0.0063). High F-PD1 expression (>33%) was seen in 14/121 (12%) and was associated with longer PFS compared to cases with ≤33% staining (2 yr PFS: 92% vs 65%, p=0.026). There was marginal association with response for CD68+ macrophages using the median of 31 cells/hpf as a cut-off: 58/65 patients (89%) with >31 cells/hpf showed a response vs 49/64 (77%) with ≤31 cells/hpf, p=0.056. The remaining IHC parameters did not show a significant correlation with response or PFS. In patients with recurrent FL (CALGB 50401), there was no association with IF-CD10 or F-PD1 staining suggesting their lack of relevance in the relapse setting, but only few high F-PD1 cases were observed. Using a biologic risk score of 1 point each for IF-CD10 positivity or F-PD1 ≤33%, untreated patients with a score of 2 had a worse PFS (median 2.9 yrs) vs those with a score of 1 (median 4.8 yrs) or 0 (median not reached), p=0.0045 (Fig 1). In multivariable Cox proportional hazards model analysis, each biologic risk factor was independent of the FLIPI risk group. Likewise, the biologic risk score was also independent of FLIPI: p=0.021, HR 0.39 (95% CI: 0.20, 0.76) for score 1 vs 2; and p=0.0005, HR 5.3 (95% CI: 1.76, 16.01) for FLIPI high vs low and HR 1.7 (95% CI: 0.59, 4.92) for FLIPI intermediate vs low, respectively.
IF-CD10 positivity appears to be a poor prognostic biomarker in FL in the untreated but not relapse setting, while high F-PD1 expression appears to be a favorable prognostic feature in untreated FL patients treated with biologic agents. These are promising biomarkers for risk stratification in FL that warrant further validation in future trials.
Support: NCI grants U10CA180821, U10CA180882
PFS in Untreated FL Patients Using a Biologic Risk Score Combining IF-CD10 and F-PD1 Expression
PFS in Untreated FL Patients Using a Biologic Risk Score Combining IF-CD10 and F-PD1 Expression
Martin:Janssen: Consultancy, Honoraria; Acerta: Consultancy; Gilead: Consultancy; Celgene: Consultancy; Novartis: Consultancy; Bayer: Consultancy. Czuczman:Immunogen: Other: Advisory board; Celgene: Employment; MorphoSys: Consultancy; Boehringer-Ingelheim: Other: Advisory Board. Bartlett:Gilead: Consultancy, Research Funding; Janssen: Research Funding; Pharmacyclics: Research Funding; Genentech: Research Funding; Pfizer: Research Funding; Novartis: Research Funding; Millennium: Research Funding; Colgene: Research Funding; Medimmune: Research Funding; Kite: Research Funding; Insight: Research Funding; Seattle Genetics: Consultancy, Research Funding; MERC: Research Funding; Dynavax: Research Funding; Idera: Research Funding; Portola: Research Funding; Bristol Meyers Squibb: Research Funding; Infinity: Research Funding; LAM Theapeutics: Research Funding. Rosenbaum:Celgene: Speakers Bureau. Leonard:Weill Cornell Medical College: Employment; Genentech: Consultancy; Medimmune: Consultancy; AstraZeneca: Consultancy; Spectrum: Consultancy; Boehringer Ingelheim: Consultancy; Vertex: Consultancy; ProNAI: Consultancy; Biotest: Consultancy; Seattle Genetics: Consultancy; Pfizer: Consultancy; Mirati Therapeutics: Consultancy; Gilead: Consultancy; Novartis: Consultancy. Cheson:Astellas: Consultancy; MedImmune: Research Funding; Teva: Research Funding; AstraZeneca: Consultancy; Ascenta: Research Funding; Pharmacyclics: Consultancy, Research Funding; Spectrum: Consultancy; Roche/Genentech: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Gilead: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal