Abstract
In the era of preemptive antiviral therapy, cytomegalovirus (CMV) still remains the cause of major health complications, profound defects in immune reconstitution, and significant morbidity in post-transplant recovery of immune-compromised HCT recipients. Substituting antivirals with a vaccine that harnesses the native immune response to CMV may improve outcomes for HCT recipients.
Modified Vaccinia Ankara (MVA), a vaccinia virus being investigated as a smallpox vaccine by the Defense Department, is a safe and robust delivery system to treat or prevent a wide range of diseases including HIV and cancer. Replication-defective MVA is safe, well tolerated and strongly immunogenic when given to HCT recipients or AIDS patients. We developed a multiple-antigen recombinant MVA with genes encoding 3 immunodominant CMV proteins: UL83 (pp65), UL123 (IE1-exon4), and UL122 (IE2-exon5) (CMV-MVA-Triplex), and established its pre-clinical safety and immunogenicity using humanized HLA transgenic mouse models and human PBMC from CMV-seropositive healthy volunteers and HCT recipients.
Defining safety, persistence of the virus, maximum tolerated dose and immunogenicity of CMV-MVA-Triplex in healthy volunteers is a critical first step in its clinical development for HCT recipients as required by the FDA. In a Phase I trial (NCT01941056), these endpoints were evaluated in 24 healthy volunteers (age: 18-60), with or without prior immunity to CMV and vaccinia. Three escalating dose levels (DL) were administered intramuscularly (DL1=10xE7; DL2=5x10E7; DL3=5x10E8 pfu/dose) in 8 subjects/DL, with a booster injection 28 days later, and follow up for 1 year.
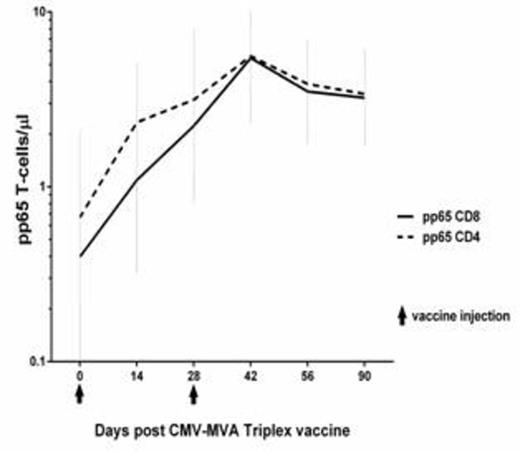
As of July 2015, all 24 planned volunteers were enrolled, vaccinated and followed for at least 4 months. Vaccinations at all DL were well-tolerated, with only a few expected injection reactions and no SAE or dose limiting toxicities. Immunogenicity of the vaccine was evaluated by measuring the levels of the CD137 T-cell surface marker representing functional activation of PBL harvested from vaccinees and stimulated 24 hours with full-length pp65, IE-1 and IE2 overlapping peptide libraries, or direct measurement of CMV-specific T-cells using HLA multimers. CMV-MVA-Triplex induced robust expansion of pp65-, IE1- and IE2-specific CD8 and CD4 T-cells in vaccinated CMV-seropositives, at each DL (Cf. plot showing geometric mean with upper lower/limits of the pp65 T-cell levels for DL2 cohort). HLA multimers identified CMV-specific T-cells whose expansion closely followed CD137-activated CMV-specific T-cells in vaccinees with common HLA alleles which have a corresponding known CMV-CTL epitope (data to be presented).
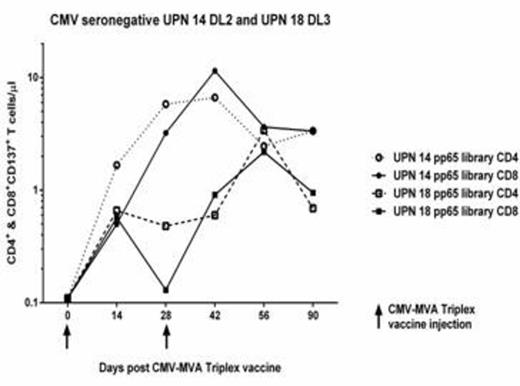
A statistical analysis performed using generalized estimated equations indicated that the post-vaccination levels of pp65-, IE1- or IE2-specific CD8 and CD4 T-cells were significantly increased, with p-values ranging from 3x10-5 to 0.025. For example, the pre-/post-vaccination median pp65-reactive CD4+ CD137+ T-cells rose from 1.3 to 4.4 cells/µL (p=3x10-5); and pp65-reactive CD8+ CD137+ T-cells rose from a median of 0.22 to 3.1 cells/µL (p=0.003). Importantly, robust immunity was detected in CMV-seronegatives (as shown in the plot for UPN 14 and 18), as well as in subjects who had received smallpox vaccinations. Elevated frequencies of CMV-specific CD4 and CD8 T cells for all 3 antigens plateaued after day 56, but in most cases remained elevated up to one year post-vaccination (data to be presented). Circulating MVA vector in blood was assessed by real-time PCR post-injection and showed only minimal residual vector DNA [10-30 gc/mL] in just 2 vaccinees in the DL3 cohort that disappeared within 3 months. These results provide evidence that CMV-seropositive HCT recipients, whether they receive stem cell product from CMV-seropositive or -seronegative donors could respond to CMV-MVA-Triplex by generating protective CMV-specific immunity.
CMV-MVA-Triplex is the first vaccine against CMV that uses a recombinant MVA incorporating multiple CMV antigens, developed for HCT recipients, who are at risk for CMV reactivation. The safety and marked immunogenicity of CMV-MVA-Triplex in this Phase I trial, warrant testing of the vaccine in the HCT setting. A Phase 2 multicenter, placebo-controlled trial to assess CMV-MVA-Triplex in CMV seropositive recipients, receiving HCT from matched related or unrelated donors will start in Fall 2015.
Diamond:Helocyte, Inc.: Consultancy, Equity Ownership, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal