Abstract
Introduction: Philadelphia-positive chronic myelogenous leukemia (CML) is a rare disease in children and constitutes approximately 3-5% of all childhood leukemias. With tyrosine kinase inhibitors (TKI), the frequency of accelerated phase (AP) or blast crisis (BC) is remarkably reduced, estimated to 1% to 1.5% per year in adults compared with more than 20% per year in the pre-TKI era. But no data are available among children.
Purpose: We described the characteristics, the treatment and the outcome of 21 children with CML, who evolved in accelerated phase and/or blast crisis under TKI.
Results: From 2001 to april 2015, 415 European patients were enrolled in the CML pediatric database. Twenty-one patients (5.1%), in chronic phase (CP) treated by TKI, presented AP or BC.
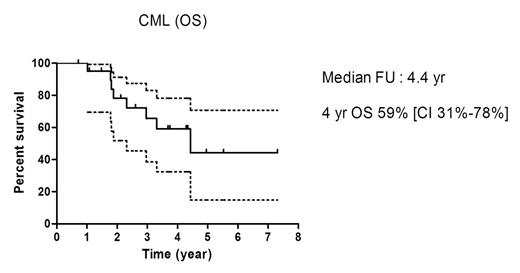
The median age of AP/BC cohort was 13.2 years (range: 4.5-16.9 years) with a sex ratio M/F at 2. At CML diagnosis, 15 patients (71%) had high risk Sokal Score with a median score of 1,4 (range: 0,16-2,4). All patients harbored t(9;22)(q34;q11) but one had a complex translocation t(1;9;22)(q12;q34;q11) and another one presented additional inv(3)(q21q26). Imatinib was the first line TKI for all patients. Before AP or BC, only five patients (24%) obtained a complete cytogenetic response (CCyR) and three achieved MMR. For incomplete molecular response or progression to accelerated phase, 8 patients (38%) were switched to dasatinib. Median duration of TKI before AP or BC was 11 months (range: 3 months-56.5 months). Six patients evolved to AP with a median interval of 8.7 months (range: 1 months-24 months), leading to blast crisis for 4 patients with a median time of 3.5 months (range: 0.3-5.4 months). Among the 2 patients remaining in AP, imatinib was increased for one and the other was switched for dasatinib, all before hematopoietic stem cells transplantation (HSCT). One patient died of post-transplant complication and the other one is still alive in complete molecular response without TKI. Nineteen patients presented BC, including 4 after AP. Thirteen patients (62%) presented ALL, five (24%) AML and one a bi phenotypic leukemia. Central nervous system (CNS) was involved for two patients with ALL, one isolated, one combined. At AP or BC, nine patients (43%) presented new additional cytogenetic abnormalities. Eighteen patients with BC were treated according to AML or ALL protocols, combined with second generation TKI for twelve patients. Only one patient underwent preparative regimen, without intensive chemotherapy before HSCT. Ten patients reached complete remission. Four patients died before HSCT, by progressive disease for 2 and by fatal infection for 2. Overall, 15 patients in BC were transplanted. Before HSCT, median molecular response was 0.2% (range: 0-29%) and only four patients had a complete molecular response. After transplant, seven patients received second generation TKI. Four patients died, including three related to transplant toxicity. Thirteen patients were alive, but one with ALL BC relapsed 26 months post-transplant and was waiting for second HSCT. With a median follow-up of 4.4 years, 4-year overall survival was 59% (66% for ALL BC versus 40% for AML BC).
Conclusion: Incidence of AP/BC after imatinib for CP CML is at 5%, in the CML pediatric database. Despite second generation TKI, combined with HSCT, outcome remains poor. Post-transplant indication of TKI is heterogenic. Recommendations would be useful for practice.
Suttorp:Novartis, Bristol Meyer Squib: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal