Abstract

Introduction: Randomized studies have demonstrated that compared to chemotherapy alone (ChemoTx), combined modality therapy (CMT) improves early event-free survival in HL patients with early stage disease. However, long-term follow up from randomized trials suggests that overall survival (OS) when receiving ChemoTx alone is equivalent or superior to OS compared with CMT. In addition, many studies have described late effects in HL survivors. While the negative impact of late-effects on LE have been estimated for pediatric HL patients (Yeh, Blood, 2012), these estimates have limited generalizability to adult HL patients due to differences in treatment regimens and exposure-related late-effects risks. To address this gap, we sought to develop an adjustable Markov model to predict LE for adult HL patients treated with contemporary therapy.
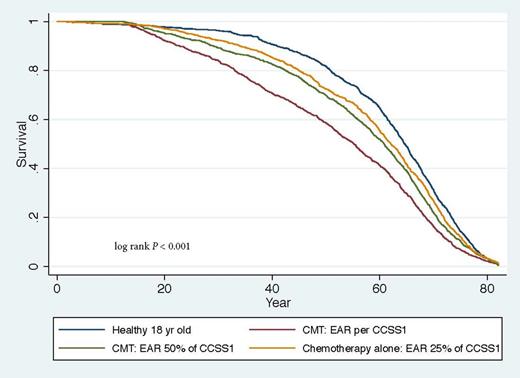
Methods: We created a Markov "state transition model" in which a cohort of patients moves through different health states. The patient cohort (base case, 18 years old) starts with initial diagnosis, and upfront treatment with 12-year OS modeled from the CCG 5942 (Wolden, JCO, 2012; COG, updated data, 2015). Following the first 12 years, the probabilities of dying were modeled by summing background mortality rates and the mortality rate associated with late effects. Background mortality rate estimates came from the 2010 CDC gender-specific LE data. Late effects mortality rates were estimated from excess absolute risk (EAR) estimates due to late effects from the Childhood Cancer Study (CCSS) Cohort 1 subjects across all disease stages who were treated with extended field RT (EFRT), higher alkylating agent therapy, and less anthracycline compared to contemporary cohorts. (Castellino, Blood, 2011) Recognizing that recent comparisons of RT doses and fields from CCSS survivors to those treated with involved field radiotherapy (IFRT) have demonstrated a reduction in RT to healthy tissues of approximately 50% (Koh, Radiation Oncology, 2007), we assumed that this RT reduction would reduce incremental mortality risk attributable to therapy by 50%. Thus, for patients treated with CMT containing IFRT, we reduced the reported EAR estimate for the CCSS-1 HL patients by 50%. Furthermore, for HL patients treated with ChemoTx alone, we assumed incremental mortality risk would be reduced by 75% (i.e., EAR reduced by 75% for this group). Because late effects mortality rates were based on pediatric data, we conducted extensive sensitivity analyses on EAR estimates to portray the scope of uncertainty surrounding LE estimates.
Results: We built on previous work on this topic by utilizing 12-year OS from CCG 5942 and by adapting data from the CCSS-1 cohort to reflect the impact of late effects on LE with more modern therapy (e.g. IFRT). 12-year OS for early stage, favorable risk HL patients treated on CCG 5942 was 98.9% and 100% for patients treated with ChemoTx and CMT, respectively. LE for an 18 year old without HL was 60.9 years. Without consideration of the burden of late effects (i.e., EAR=0), a patient with early stage, favorable risk HL had a LE similar to a healthy 18 year old without HL. For HL patients, LE with ChemoTx alone (base case, COPP/ABV) was 58.0 years and the LE for treatment with CMT (i.e., COPP/ABV + IFRT) was 55.7 years. Additionally, reduced LE was also apparent for HL patients who received ChemoTx alone (see Figure). Finally, in order to apply these data to individual HL patients, we created an adjustable model with variables including age, gender, risk group (favorable/unfavorable), and gender- and treatment-specific EAR that may potentially be applied to an individual HL patient.
Conclusion: We created an adjustable Markov model that predicts LE for adult HL patients treated with contemporary therapy. This model, including longer term OS data, demonstrated that contemporary therapy reduces the late effects burden. However, for survivors of early stage HL, we found that LE loss due to late effects substantially exceeds LE loss due to HL. To further enhance this model for the potential application in adults with HL, further synthesis of available pediatric and adult data (accounting for contemporary therapy) is needed to account for differences in EAR by age and gender over a life span. Altogether, models that synthesize clinical trial data provide valuable information to providers and may help guide them and HL patients towards individualized therapeutic decisions.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal