Abstract
Background
The relevance of differential splicing in human cancer is an evolving area of cancer biology. The recent findings of frequent mutations of the splicing pathways in MDS provide insight into the mechanism of alternative splicing, which has been long associated with the development of cancer. The genome-wide microarray analysis using Exon arrays discovered significantly differentially spliced genes in AML. Moreover, the AML specific "splicing profile" was normalized in remission and reappears with patient relapse, thereby supporting a role of deregulated splice variants in the process of leukemogenesis.
A close cytogenetic and molecular analogy between de novo MDS and AML of elderly people suggests a common pathogenic mechanism for these conditions. Recent clinical and biological studies indicate that MDS and AML could be considered as part of the same continuous disease spectrum rather than as distinct disorders. Recently, we found that high expression of the NPM1 splice variant R2 may provide prognostic value for CN-AML patients. Assuming the common origin of MDS and AML we aimed to characterize the NPM1 R2 splice variant expression as well as the influence of R2 expression on NPM1 localization in groups with MDS, sAML and AML patients. Moreover, NPM1 stabilizes the ARF and interacts with the tumor suppressor p53, regulates the increase in stability and transcriptional activation of p53, thus contributing to modulating growth-suppressive pathways. Therefore, we characterized expression pattern of ARF, MDM2, TP53 genes with additional downstream molecules (p21, miR-34a) in AML, s-AML and MDS patients.
Methods
Since we found prognostic significance of the expression level of R2 for the AML cohort of patients, therefore we decided to evaluate its significance for MDS and sAML cases. For 61 samples (25 AML, 30 MDS and 6 samples with sAML) qRT-PCR was performed. Expression level of NPM1 R2 was assessed. To investigate whether R2 might disrupt localization of the NPM1 wild type protein, immunohistochemistry analysis for NPM1 in 23 AML bone marrow smears was performed. As NPM1 contributes to regulation of ARF-MDM2-p53-p21 signaling pathway proteins we assessed if high or low expression of its splice variant R2 might have influence on expression pattern of these transcripts.
Results
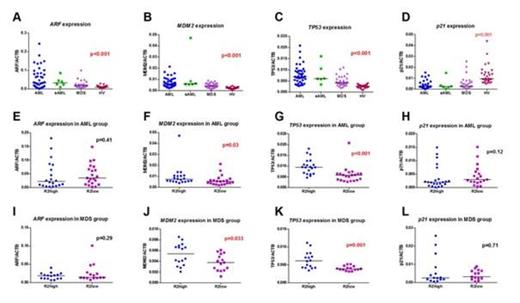
The expression of R2 was significantly higher in AML, s-AML and MDS groups compared to HVs (median 0.022 vs 0.005, p<0.001, 0.022 vs 0.005, p<0.001 and 0.015 vs 0.005, p<0.001, respectively). The IHC stainings for AML samples revealed that in cases with high R2 expression we were able to determine a cytoplasmic localization of NPM1 even in the absence of its concomitant mutation. Therefore, we provide further evidence that the cytoplasmic localization of NPM1 might depend not only on its mutational status, but might be influenced by the distribution of its splice variants. We performed ARF, MDM2, TP53 and p21 mRNA expression analysis in AML, s-AML, MDS and HV groups and found significant differences between these groups (Figure 1A-D). We also analyzed the expression of ARF, MDM2, TP53 and p21 in groups with high or low R2 expression. We found elevated expression of MDM2 and TP53 in groups with high R2 expression in comparison to groups with low R2 expression in AML patients (median 0.007 vs 0.005, p=0.03 and 0.009 vs 0.005, p<0.001, respectively), (Figure 1F, G). In case of MDS patients we also found elevated expression of MDM2 and TP53 in groups with high R2 expression compared to groups with low R2 expression (median 0.005 vs 0.003, p=0.033 and 0.006 vs 0.003, p=0.001, respectively), (Figure 1J, K).
Conclusions
In our study we found that the expression levels of R2 were elevated in AML, sAML and MDS groups compared to HVs suggesting that R2 might play some role in the process of the tumorigenesis not only in AML cases but also in early stages of development of this disease. As the NPM1 R2 splice variant represents a truncated form of NPM1 gene this isoform mostly localizes in the nucleoplasm, and thus might also have a biological impact in the malignant cells. We found elevated expression of MDM2 and TP53 in groups with high R2 expression compared to groups with low R2 expression in AML as well as MDS patients. In summary, the expression of NPM1 R2 might be of biological importance for AML as well as for sAML and MDS patients.
This work was supported by National Centre for Science Grant HARMONIA (UMO-2013/10/M/NZ5/00313).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal