Abstract
Introduction
Treatment of elderly patients with acute myeloid leukemia (AML) is a therapeutic challenge. Elderly patients frequently have more biologically inherent resistant disease, along with comorbidities that together result in poor overall survival (OS). Optimal frontline therapy for elderly patients with AML remains controversial, and choice of regimen varies among clinicians. In this large, single-institution retrospective cohort study of AML patients over age 70, we present survival analysis and comparison amongst a variety of commonly used initial regimens.
Methods
602 AML patients aged 70 or greater who received treatment between 1995 and 2014 in a single-large institution were retrospectively analyzed. Patients were categorized into 4 different treatment groups: High Intensity Therapy (defined as daunorubicin/cytarabine or equivalent), Hypomethylating Agent (HMA) Therapy, Low intensity Therapy (defined as low-dose cytarabine or similar without HMAs), and Supportive Care (including hydroxyurea if indicated). Age, type of AML, history of previous hematological disease, cytogenetics, ECOG performance status, comorbidities (Charlson Index), complete blood counts and blast percentage at time of diagnosis were obtained for each treatment category. Pairwise comparison of survival between different treatment groups was performed, using the stratified log-rank test and propensity score matching to adjust for potential treatment indication bias between groups. Within pairwise comparison groups, the stratified Cox proportional hazards regression model was used to assess correlation of the clinical variables with overall survival.
Results
Median age was 77 years (range 70 - 95) with a male predominance (M:F=68%:32%). ECOG Performance Status was 0 to 1 in 80% and 2 to 4 in 20% of patients. Per NCCN criteria, cytogenetics risk category was intermediate or favorable in 67% and unfavorable in 33%. Baseline median WBC, hemoglobin and platelet counts were 3.31 k/uL, 9.40 g/dL and 43 k/uL respectively. Median baseline bone marrow blast percentage was 35% (range 2% - 95%), and the large majority (445 of 550 patients - 81%) had peripheral blood blasts at the time of diagnosis. The majority of patients had secondary AML (61%) compared with de novo AML (39%). Of those with secondary AML, myelodysplastic syndrome (MDS) was the most common antecedent hematologic disease (97%), for which 36% had received prior HMAs.
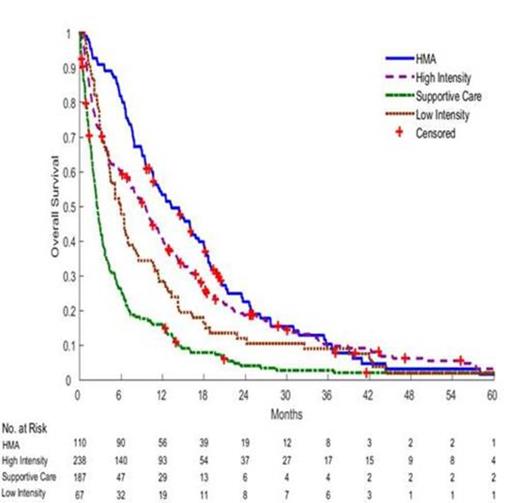
For frontline therapy, 238 (40%) patients received High Intensity Therapy; 110 (18%) received HMA Therapy, 67 (11%) received Low Intensity Therapy, and 187 (31%) received Supportive Care. Pairwise comparison between HMA Therapy and the 3 other treatment groups individually demonstrated statistically significant superior OS with HMA Therapy (median 13.3 mo; 95% CI 10.6 - 16.8 mo) compared to High Intensity Therapy (median 9.5 mo; 95% CI 7.4 - 10.9 mo), Low Intensity Therapy (median 5.9 mo; 95% CI 4.2 - 7.8 mo) and Supportive Care (median 2.5 mo; 95% CI 2.1 - 3.0 mo.). In addition, pairwise comparisons demonstrated superior OS with high vs low-intensity (p=0.0007), but no significant difference between Low-Intensity and Supportive Care (p=0.10). A pairwise comparison between HMA and High Intensity Therapy in the small subset of patients who had received prior HMA for MDS revealed extremely poor outcomes in both arms, with < 6 month median OS.
Conclusion
In this analysis of a very large data set of patients over age 70 with AML, using pairwise comparison with propensity score matching, our results indicate a survival benefit with high intensity therapy or HMAs compared to supportive care or low-intensity (non-HMA) therapy. Interestingly, treatment with HMAs also resulted in better OS than traditional high intensity therapy. These data are contributing to an ongoing effort to design a comprehensive decision analysis model comparing treatment effectiveness according to baseline characteristics in AML patients 70 and older.
Overall Survival Amongst Treatment Groups
Lancet:Kalo-Bios: Consultancy; Boehringer-Ingelheim: Consultancy; Celgene: Consultancy, Research Funding; Amgen: Consultancy; Seattle Genetics: Consultancy; Pfizer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal